EKG Interpretation for Nurses | NURSING.com
Interpret EKGs Strips Like a Boss!
You aren’t the only one that’s a bit terrified of EKGs . . . let’s just clear that up right away. For many nursing students and new nurses, EKG interpretation can be intimidating, to say the least. I remember my first day as a nurse in the ICU . . . monitors were EVERYWHERE. To say that I was overwhelmed is a pretty big understatement.

But the truth is you don’t have to be so scared. In fact, you can interpret ANY heart rhythm in just 5 simple steps. Let me warn you though that you have to follow these steps EXACTLY you can’t skip ahead, you must follow these steps in order.
- Free EKG Cheatsheet: Click to Get our Book “EKG Interpretation”
- EKG Course: View NURSING.com EKG Course
5 Steps to EKG Interpretation
- Rate
- P Waves
- P:QRS
- QRS
- PR Interval
 Step 1: Rate
Step 1: Rate
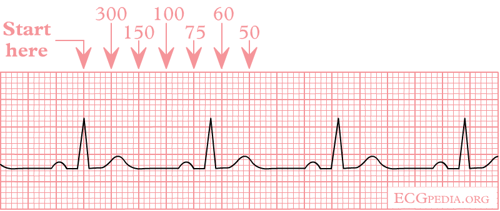
- What is the ventricular rate?
- On a six second strip count the R waves and multiply by 10
- Alternatively, you can divide 300 by the number of large squares between R waves or P waves. This method is less reliably if the rate is irregular.
Step 2: P Waves
- Are there P Waves?
- What is the rate of the P wave?
- What is the morphology of the P wave (upward, smooth, rounded)?
Step 3: P:QRS
- Is there a 1:1 relationship between P wave and QRS complex?
Step 4: QRS
- Are there QRS complexes?
- Is the QRS width 0.06 – 0.12 seconds (1.5 – 3 small boxes)?
Step 5: PR Interval
- Is the PRI between 0.12 – 0.20 seconds (3 – 5 small boxes)?
Normal Sinus Rhythm
Rate
- 60 – 100 bpm
P Waves
- Are there P Waves?
- Yes
- What is the rate of the P wave?
- 60 – 100
- What is the morphology of the P wave (is it positive, smooth, or round)?
- Yes
P: QRS
- Is there a 1:1 relationship between P wave and QRS complex?
- Yes
QRS
- Are there QRS complexes?
- Yes
- Is the QRS width 0.06 – 0.12 seconds (1.5 – 3 small boxes)?
- Yes
PR Interval
- Is the PRI between 0.12 – 0.20 seconds (3 – 5 small boxes)?
- Yes
Explanation:
Normal sinus rhythm is the result of the electrical conduction following the intended course without deviation or alteration in rate. Slight variations in rhythm regularity may be noted with the respiratory cycle.
Now What?
Okay. . . at this point you should have a basic grasp of how to identify and interpret normal sinus rhythm. This is the BEST place to start. But this is just the beginning. In order to become an EKG master, you need to become comfortable with a wide range of rhythms. Let's dive into how to interpret different rhythms.
Bradycardia
- There are two types of bradycardia:
- Sinus bradycardia
- Atrioventricular (AV) block
- First degree
- Second degree
- Type 1 (Wenckebach)
- Type 2 (Mobitz)
- Third-degree (complete)
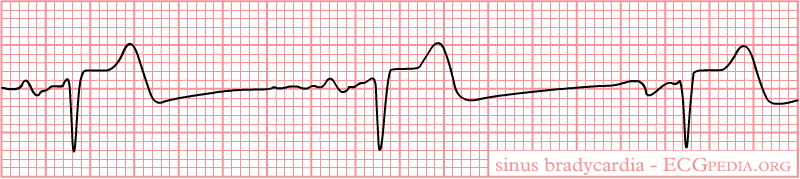
Sinus Bradycardia EKG Interpretation
When looking at an EKG that is sinus brady, all PQRST waves are within normal measurements meaning that the PR, QRS, and QT intervals all meet the criteria for sinus rhythm. However, when you count out the heart rate it is less than 60 bpm.
What causes Sinus Bradycardia?
Sinus bradycardia can be seen in healthy adults if they are athletic and/or are asleep! Other common causes of sinus brady include:
- Heart tissue damage
- Hypertension
- Myocarditis
- Hypothyroidism
- Lupus
- Common with inferior wall MI
- Increased ICP
- Increased vagal tone from vomiting
- Bearing down to have a bowel movement
- Hemochromatosis
- Medications:
- Heart rhythm/Hypertensive medications Beta-blockers
Nursing Mnemonic For Causes of Bradycardia
PACED
-
- Propranolol or Poppies (Opiates)
- Anticholinesterase drugs
- Clonidine or Calcium Channel Blockers
- Ethanol
- Digoxin
What could happen to someone in sinus bradycardia?
Patients with sinus bradycardia will likely be asymptomatic, however, it makes sense for patients to exhibit signs and symptoms of cardiac compromise such as:
- Altered LOC
- Hypotension
- Respiratory distress/failure
- Delayed capillary refill
- Syncope
- Shortness of breath (SOB)
How do you treat bradycardia?
- Medications:
- First line:
- Atropine
- Second line:
- Dopamine
- Epinephrine
- First line:
Transcutaneous pacing should be used if the patient is exhibiting signs and symptoms of poor profusion.
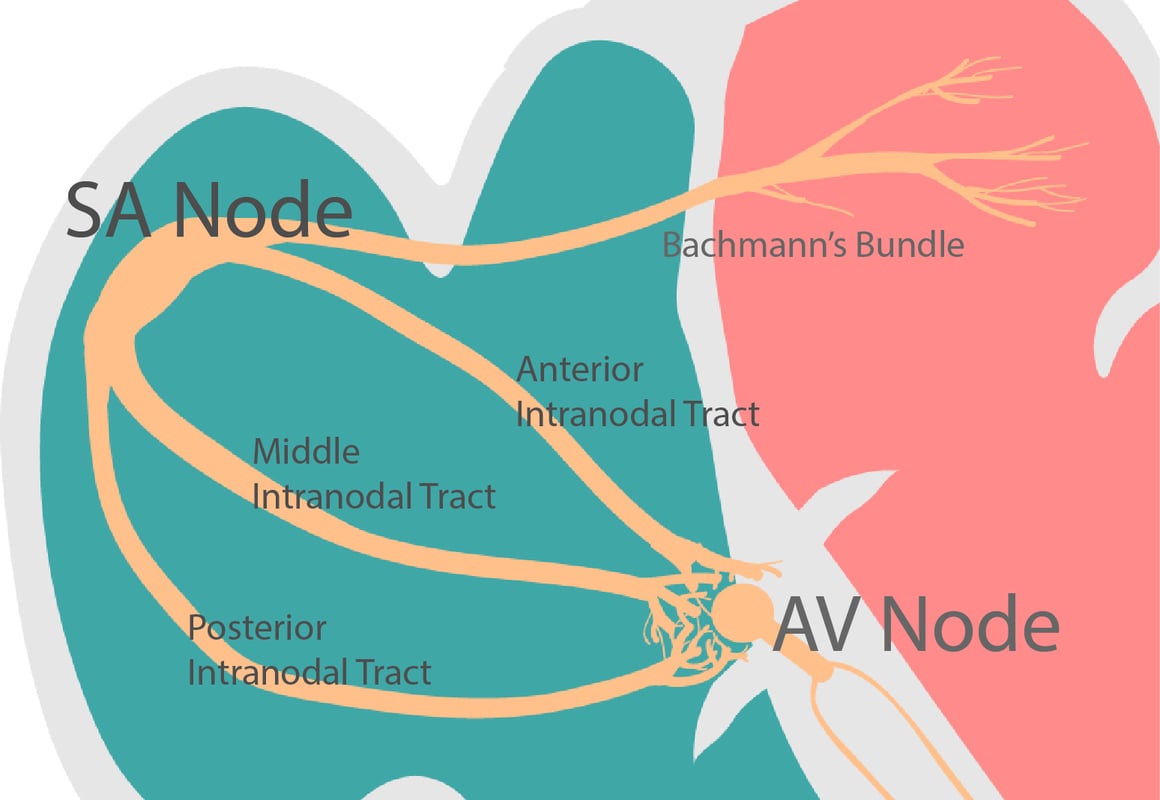
AV Blocks
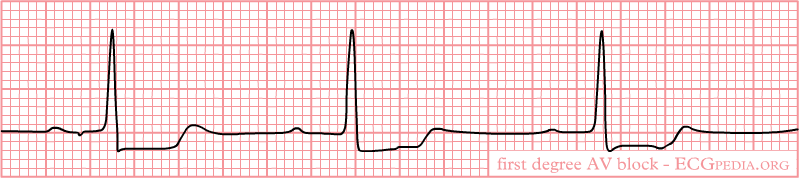
- First degree:
- This is the mildest form of the heart blocks and is rarely symptomatic. There are very few times this rhythm will receive treatment. The electrical signals from the atria to the ventricles are delayed, causing long PR intervals.
- Second degree:
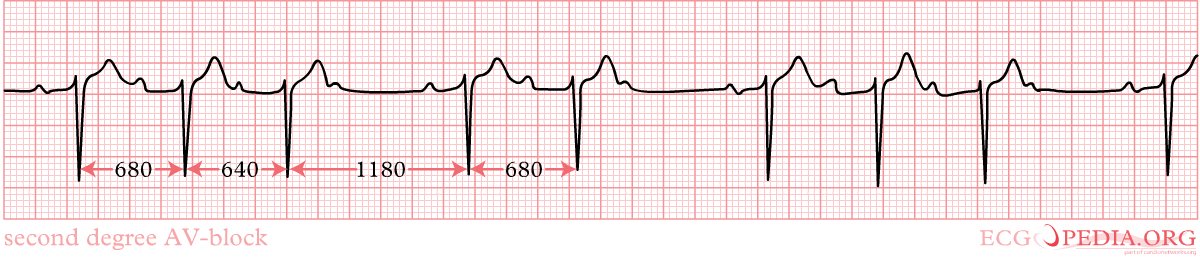
- In second degree AV block, not all electrical signals reach the ventricles causing some beats to drop as well as causing an irregular rhythm., There are two types of second degree block:
- Type 1 which is also called Wenckebach
- In second degree type 1 AV block, the atria are pumping at a regular rate but ventricles are pumping slower causing prolonged regular PR intervals.
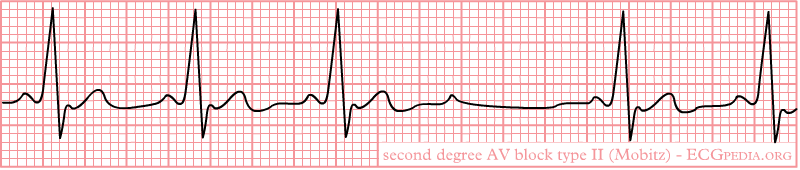
- Type 2 which is also called Mobitz
- In second degree type 2 AV block, the conduction delay is below the AV node. Thus, the SA node is firing regularly causing regular P to P waves but either bundle of his or bundle branches are not receiving the action potential every time causing skipped QRS complexes.
- Type 1 which is also called Wenckebach
- In second degree AV block, not all electrical signals reach the ventricles causing some beats to drop as well as causing an irregular rhythm., There are two types of second degree block:
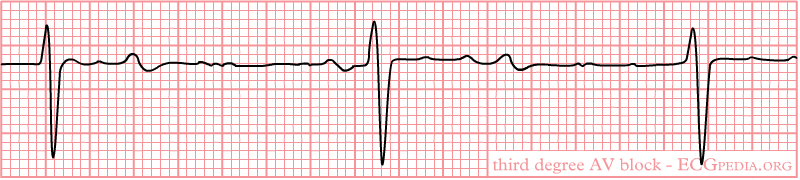
- Third degree which is also called complete
- In third degree AV block, the atria and ventricles are not communicating at all… Communication is “blocked” you might say! The atria are using their pacemaker, the Sinoatrial (SA) node, which beats at 60-80 bpm, but since the conduction pathways for the electrical signal to pass on to the ventricles are blocked, the ventricles use their own intrinsic pacemaker. This can either be the junction (40-60 bpm) or bundles (20-40 bpm). This chaotic messaging system can cause P waves to happen in the middle of a QRS complex. Because the P waves represent the atria pumping and the QRS complex represent the ventricles pumping and the atria are receiving almost double the amount of signals, there will be more P waves than QRS waves.
Recognizing AV block bradycardia on an EKG
- First degree
- PR interval consistently greater than 20
- Less than 60 bpm
- Regular rate
- Second degree
- Type 1 (Wenckebach)
- P to P intervals are regular
- PR intervals become progressively longer
- Eventually a QRS complex is skipped
- Type 1 (Wenckebach)
- Type 2 (Mobitz)
- P to P intervals are regular
- Extra P waves (no QRS complex to follow)
- PR intervals are regular when there is a QRS complex following that P wave
- Has the potential to progress to complete heart block
- Third degree (complete)
- P waves continue to be 60-80 bpm
- QRS complexes are at the rate of either 40-60 bpm or 20-40 bpm
What causes AV block?
First degree AV block, second degree type 1 AV block, and third degree AV block can be caused by the following issues:
- Acute inferior MI
- Right Ventricular infarction
- Increased vagal tone
- Ischemic heart disease
- Digitalis toxicity
- Beta blockers
- Amiodarone
- Calcium channel blockers
- Electrolyte imbalances
- Rheumatic heart disease
- myocarditis
Second degree type 2 (Mobitz), however, is caused by damage to the bundle branch system following an acute anterior Myocardial infarction. It is important to note that second degree type 2 AV block is NOT caused by medications or increased vagal tone.
What can happen to a patient in AV block?
AV blocks are usually asymptomatic. However, a patient may experience the following:
- Fainting/syncope
- Heart failure
- Cardiac arrest and death
- Hypotension
How do you treat AV block?
The main goal of treating AV block usually depends on if the patient is symptomatic or not. If they are not symptomatic and their heart rate is sustaining appropriate profusion, then the goal is to monitor PR intervals and make sure that the heart block conduction system does not worsen. In each specific degree of heart block, you will want to follow the following:
- In first degree AV block, you want to holding medications that cause slow AV conduction and monitor for lengthening PR intervals
- In second degree AV block type 1, also called Wenckebach, if the patient is too bradycardic, you will give them atropine and possibly use pacing, but only temporarily. The best outcome is if the cause of the heart block is discovered and that underlying cause can be treated. It is important to monitor for progression into higher forms of block
- In second degree type 2 AV block, also called Mobitz, if the patient is symptomatic, you will use a transcutaneous pacer and dopamine for hypotension. If the patient is asymptomatic but not maintaining proper profusion, you will have the transcutaneous pacer nearby and ready to use. You will also want to hold all drugs that slow the AV node conduction.
- In third degree AV heart block, also called complete heart block,a symptomatic patient who is bradycardic will need to receive atropine as well as being paced by a transcutaneous pacer.
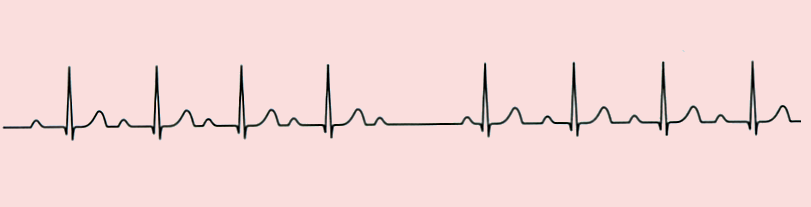
Sinus Tachycardia EKG Interpretation
On the EKG, all PQRST wave forms present and the rhythm is regular, just very fast. 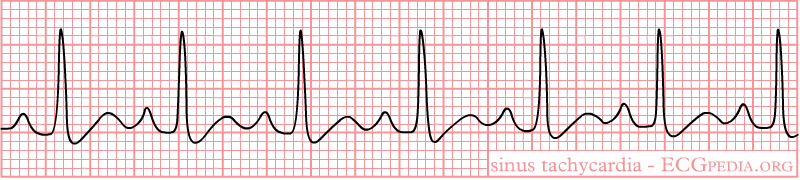
What causes Sinus Tachycardia?
- Heart tissue damage
- Heart attack
- Heart failure
- Abnormal vital signs:
- Fever
- Hypertension
- Pain
- Stress/anxiety/fear
- Alcohol, caffeine, nicotine
- Cocaine
- Electrolyte imbalance
- Hyperthyroidism
- Anemia
- Hemorrhage
What could happen to someone in Sinus Tachycardia?
Sinus Tachycardia causes decreased cardiac output due to inadequate ventricular filling as well as an increased oxygen demand for the myocardial cells. A patient with sinus tachycardia may have the following signs and symptoms:
- Dizziness
- Lightheadedness
- Syncope
- Chest Pain
- Fast heart rate
- Palpitations
- Shortness of breath
How do you treat Sinus Tachycardia?
The best treatment for sinus tachycardia is to treat the underlying cause. If a patient has a fever, administer antipyretics such as Motrin or Tylenol, or if they have anxiety give them an anti-anxiety medication such as Xanax, Valium or Ativan. If the patient has a narrow QRS complex, then treat them with the following:
If the patient has a wide QRS complex, then treat them with an antiarrhythmic such as Procainamide, Amiodarone, or Sotalol.
Closer Look at Atrial Rhythms
Let’s look even closer at Atrial Rhythms. When the sinoatrial (SA) node is not generating proper electrical activity, the hearts atrial tissues or even other tissues of the heart will attempt to generate electrical action potential. This can cause issues with the heart not beating properly, completely, or rhythmically. Watch this video below:
What is PSVT?
Paroxysmal Supraventricular Tachycardia (PSVT) is a rapid heartbeat that originates in the atria. It is called paroxysmal because it happened intermittently and lasts various lengths of time. PSVT is often just called SVT.
Recognizing PSVT on an EKG
The EKG will show a fast heart rate anywhere from 100 to up to 300 bpm! The QRS is narrow at a regular rhythm. Sometimes the P waves are inverted, this is referred to as retrograde P waves. 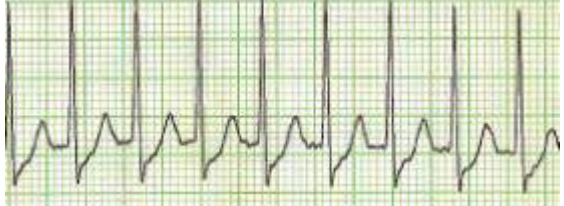
What causes PSVT?
A patient can be genetically inclined to have PSVT; Their electrical conduction doesn’t fire normally. It can also be drug-induced; Digoxin and Theophylline can cause PSVT. However, certain behaviors such as alcoholism, caffeine, drug use, or smoking can put you at risk as well.
- Signs and symptoms:
- Anxiety
- Shortness of breath
- Tachycardia
- Palpitations
- Dizziness
- Syncope
What could happen to someone in PSVT?
Patients who have sustained PSVT can have adverse effects such as hypotension due to the inevitable incomplete heartbeats from the fast beating of the heart. As well as over time, the heart will enlarge (Cardiomegaly) and eventually fail (heart failure).
How do you treat PSVT?
Because PSVT can be treated by the patient by themselves, the first line of treatment involves performing the Valsalva maneuver where the patient holds their breath and bear down as if they were having a bowel movement, or cold water on the face (splashing or submerging). Coughing while positioned sitting forward can also bring someone out of PSVT. In the hospital, a patient may get a carotid massage by a physician, medications such as adenosine (Adenocard) and cardioversion.

- Paroxysmal Afib (early)
- Usually when first diagnosed
- Periods of Afib that come and go
- Afib usually goes away on its own
- Persistent Afib
- Medications are needed to correct Afib (we will talk about medications later)
- Longer and more frequent episodes of Afib
- Permanent Afib (late)
- Have had Afib for a long time and the heart is unable to return to Normal Sinus Rhythm (NSR).
AFib EKG Interpretation
The waves are more chaotic and random, the beat is irregular and you can see the atria quivering between the QRS (ventricles pumping). No discernible P waves. The ventricular rate is often 110-160 bpm and the QRS complexes is usually less than 120 ms. 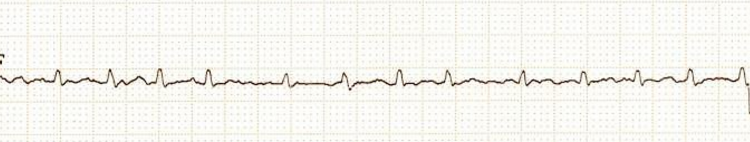
What causes Afib?
The actual cause of Afib is unknown but research suggests many risk factors that are commonly seen with patients with Afib.
- Risk factors
- Age
- Family history
- Smoking
- Hypertension
- Obesity
- Conditions increasing risk
- Heart failure
- Diabetes
- Coronary heart disease
What could happen to someone in Afib?
Due to the pooling of blood from incomplete contractions and the quivering of the atria, a patient is likely to form a clot. If the blood clot breaks free it can cause a stroke or pulmonary embolism (PE) and increase the risk of heart failure and death. A patient with Afib may not have any signs or symptoms at all (about 60% do not), however, a patient may feel lightheaded, dizzy, short of breath, as well as experience chest pains, palpitations, and/or weakness. Afib also causes the heart to undergo a process called remodeling where the walls thicken and the heart size increases.
How do you treat Afib?
The two main goals of treating Afib is controlling the rate and rhythm and prevention of stroke/pulmonary embolism (PE). Medications can be used to control a patient's rate and rhythm. The most commonly used medication for the rate is adenosine. The two most commonly used medications for rhythm control are diltiazem (Cardizem) and amiodarone (Cordarone). Cardizem is better at controlling the rhythm but can cause hypotension in the patient, whereas amiodarone is better for hemodynamically compromised patients. Anticoagulants are used for stroke and pulmonary emboli prevention. Heparin is the first line, however, Lovenox and warfarin (Coumadin) are also used. If medication has not been successful in controlling the rate or rhythm, the patient may have a medical procedure to correct this arrhythmia.
- Cardioversion
- Electrical current is used to restore electrical heart rhythm
- Surgical ablation
- Destroys the cells that are causing abnormal heart rhythm
- Catheter ablation (radiofrequency ablation)
- Stops the heart from setting off the faulty electrical signals
- Atrial Pacemaker
- Placed under the skin to generate electrical signals to regulate heartbeat
Recognizing AFlutter on an EKG
This was always the easiest rhythm for me to pick out because it is so unique. The jagged edges are similar to that of a saw blade, and people refer to it as a saw tooth pattern. The rate is regular but fast. 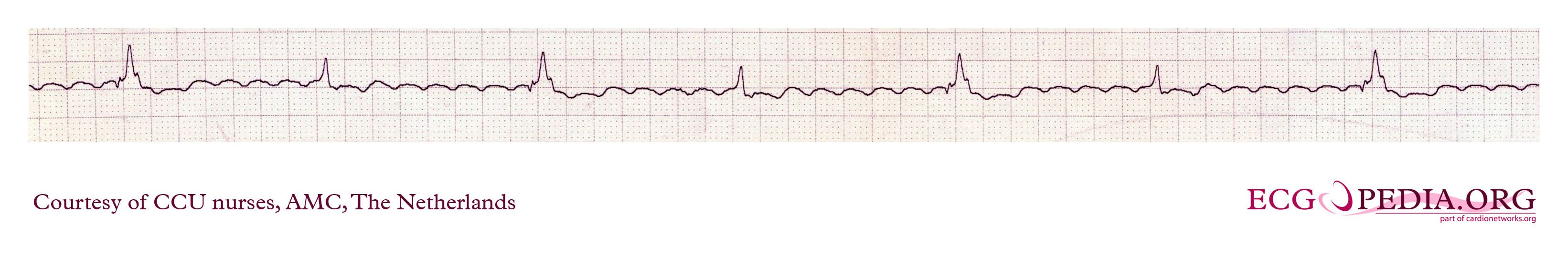
What causes AFlutter?
- Heart conditions:
- Rheumatic or ischemic heart disease
- Heart failure
- Previous heart attack
- Pericarditis
- Septal defects
- Hypertension
- Pre-excitation syndromes
- Atrioventricular (AV) valve disease
- Non-cardiac conditions:
- Thyroid dysfunction (hyperthyroidism, thyrotoxicosis)
- Too many thyroid hormones cause electrical changes within atrial myocytes, shortening the action potential
- Diabetes
- Fluctuations of serum glucose can cause the increased size of the atria, leading to electrical conduction problems.
- Alcoholism
- Shortens the right atrial effective refractory period (AERP)
- Thyroid dysfunction (hyperthyroidism, thyrotoxicosis)
What could happen to someone in AFlutter?
- Signs and symtpoms
- Palpitations
- Fast steady heart beat
- Shortness of breath (especially upon exertion)
- Anxiety/Nervousness
- Chest pain
- Dizziness
- Lightheadedness
- Syncope
If untreated can lead to cardiomyopathy, heart failure, and Afib.
How do you treat AFlutter?
Generally speaking, AFlutter itself isn’t life-threatening, however, long term, it can cause complications similar to Afib. The most common treatment for Aflutter is cardioversion and medications.
- Medications
- Ibutilide (Corvert)
- Give to patients before cardioversion
- Amiodarone (Coradarone)
- Diltiazem (Cardizem)
- Ibutilide (Corvert)
- Severely compromised
- Cardioversion (treatment of choice)
- Rapid atrial overdrive pacing
- Radiofrequency catheter ablation
- Monomorphic: QRS’s are the same size
- Polymorphic: QRS’s are different size and shape
Recognizing VTach on an EKG
The rhythm is regular but the rate is fast (above 100 bpm). The QRS complex is widened and P waves can be difficult to identify. This is a very easy rhythm to glance at and interpret due to its characteristic waves. 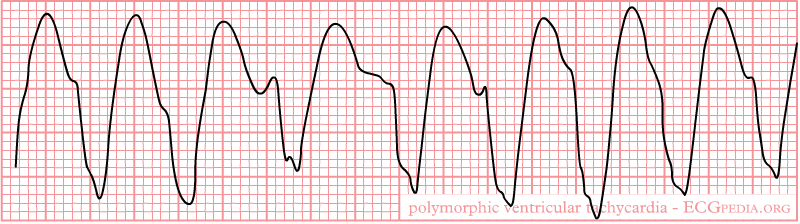
What causes VTach?
VTach can occur in patients who have heart diseases such as:
- Cardiomyopathy
- Heart failure
- Heart surgery
- Myocarditis
- Valvular heart disease
And can be present due to abnormal blood conditions such as:
What could happen to someone in VTach?
A patient with VTach could be asymptomatic, however, signs and symptoms include:
- Signs and symptoms
- Dizziness
- Lightheadedness
- Palpitations
- Shortness of breath
- Chest pain
- Syncope
- Loss of consciousness
If left untreated, VTach can cause sudden cardiac death
How do you treat VTach?
The most immediate goal is to slow the heart rate. This is managed through medications (such as Lidocaine, Procainamide, Sotalol, or Amiodarone), defibrillation and possible cardiopulmonary resuscitation (CPR). Chronic long term VTach is treated with an implantable cardioverter defibrillator (ICD).
Recognizing V.Fib on an EKG
VFib is easily recognized because of its rapid, chaotic, and irregular nature. The QRS complexes are variable in height and width as well as there are no P waves. 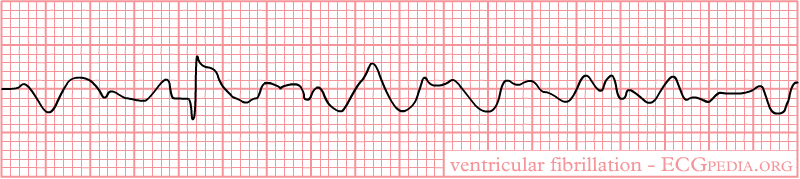
What causes V.Fib?
VFib can be caused by:
- acute myocardial infarction
- trauma
- drug overdose such as heroin
- electrolyte imbalances
Ventricular tachycardia will become ventricular fibrillation if it is left untreated. Electrolyte imbalances also can cause VFib because our muscles (the heart is a giant muscle) uses calcium (Ca-) and potassium (K+) to contract and magnesium (Mg) to relax.
What could happen to someone in V.Fib?
Your patient will likely lose consciousness and they will not have a pulse. VFib needs to be recognized and treated immediately because it leads to cardiac arrest and death.
EKG FAQ’s
How do you read an ekg strip?
By looking at the waveforms on the EKG graph you look for the P wave followed by the QRS wave and T wave in that specific order.
How to measure an ekg strip?
Each small box is 0.04 seconds and each large box is 0.20 seconds. There are 5 small boxes in a large box (0.04 X 5 = 0.20 seconds).
How many seconds is an ekg strip?
Most EKG strips are 6 seconds, the graph paper has a marking on the top or bottom to indicate every 3 seconds. You can also count the large boxes, 30 large boxes equal 6 seconds, most 12 lead EKGs are 10 seconds long.
What does an abnormal EKG strip look like?
An abnormal EKG strip will not follow the traditional P wave, QRS wave, and T wave order. There could be an additional P wave or an extra QRS complex or an irregular rhythm.
How to calculate a heart rate on an EKG strip?
By counting the R waves on a 6-second strip and multiplying by 10. You can count the small boxes between the R waves and divide 1500 by the number of R waves (1500/20 = 75). Or you can count the large boxes
How do you treat V. Fib?
This is the time you call a code blue, grab the crash cart, and get on the patients’ chest. With VFib, it is super important to defibrillate as soon as possible. For further details about running a code, check out the ACLS algorithm. Check out this awesome website for more helpful information about cardiac rhythms!
3 Common EKG Changes and Nursing Interventions
When you’re taking care of patients on cardiac monitoring, It’s important to be able to not only identify rhythm changes but also have an idea of some typical interventions for these changes. I’m going to go over a few common ECG changes and typical subsequent nursing interventions.
Cardiac Monitoring Equipment Basics for Nursing Students
Pacemaker Considerations During Cardiac Monitoring
Identify ANY EKG Rhythm in 10 Seconds or Less
The 5-step method for rapid EKG interpretation outlines the steps to help you quickly spot arrhythmias with confidence. There are many more factors involved in fully understanding EKGs but this simple 5 step method will help you know exactly where to start. If you work through the 5 steps in order you will be able to look at any strip and quickly notice abnormalities. You can view a PDF chart with essential heart rhythms and their criteria here.
- Rate
- P Wave
- QRS Complex
- P:QRS
- PR – Interval
Rate
With any strip, you should start with the rate which can be determined (on a 6-second strip) by counting the P waves or the R waves and multiplying by 10. You can also count the number of large boxes between R waves and divide 300 by that number. For example, if you count 5 large boxes between each R wave then your rate would be approximately 60 bpm. Identifying the rate is a good way to determine where the impulse is initiating and can quickly rule out sinus rhythm.
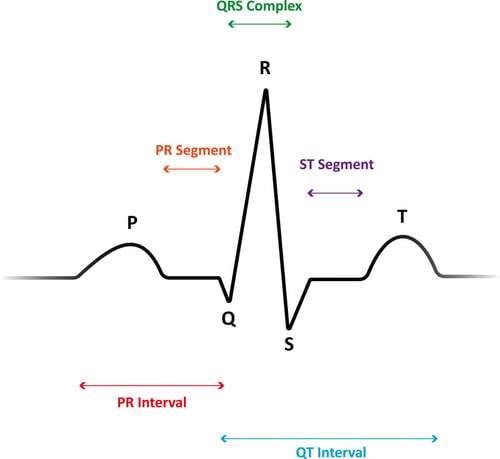
P Wave
The P wave is representative of atrial depolarization and the wave should have an upward direction, it should be visible, and smooth. If you do not see P waves or they are misshapen you are not dealing with sinus rhythm.
QRS Complex
The QRS complex represents ventricular depolarization and should be present. The complex should have a length of 0.06 – 0.12 seconds (1.5 – 3 small squares). Anything out of this range is abnormal.
P:QRS
Every P wave should be followed directly by a QRS. The ratio between P and QRS should be 1:1. This represents the appropriate route of impulse travel. Deviation or alteration from the impulse traveling from SA node through Purkenji fibers in the right direction may be identified with the P:QRS.
PR Interval
The PR interval represents the onset of atrial depolarization and the onset of ventricular depolarization and is a factor in determining how long the impulse is held in the AV node. PR interval analysis is helpful in identifying AV heart blocks. The PR interval should be between 0.12 – 0.20 seconds (3 – 5 small squares).
EKG FAQ:
By looking at the waveforms on the EKG graph you look for the P wave followed by the QRS wave and T wave in that specific order.
Each small box is 0.04 seconds and each large box is 0.20 seconds. There are 5 small boxes in a large box (0.04 X 5 = 0.20 seconds).
Most EKG strips are 6 seconds, the graph paper has a marking on the top or bottom to indicate every 3 seconds. You can also count the large boxes, 30 large boxes equal 6 seconds, and most 12 lead EKGs are 10 seconds long.
An abnormal EKG strip will not follow the traditional P wave, QRS wave, and T wave order. There could be an additional P wave or an extra QRS complex or an irregular rhythm.
By counting the R waves on a 6-second strip and multiplying by 10. You can count the small boxes between the R waves and divide 1500 by the number of R waves (1500/20 = 75). Or you can count the large boxes