Nursing Dosage Med Math Calculations | NURSING.com

Everything dosage calculations and dimensional analysis . . . with practice
One of the most stressful parts of nursing school is nursing med math and dosage calculations . . .
Try a Dimensional Analysis Question NowIn this post, we are going to provide you with EVERYTHING you need to simplify med math.
When I was in school (2007-2010), we had a nursing math test each semester. We had to get at least a 96% or we failed the nursing math test, and if we did that… we failed the course.
Pretty brutal.
It’s stressful to have that in your mind while taking these tests… but what may be even more stressful is knowing that you’re calculating medications for patients and if you’re way off, it could result in bad news bears for your patient.
At NURSING.com, we completely feel your pain. We were there. We had to take and pass many math classes throughout nursing school. We also had to take and pass the ever-painful pharmacology course as well. Med math for nurses and pharmacology absolutely go hand-in-hand, and we know this connection is so important that we created a course to help you not only get through pharmacology but truly understand it. Our Nursing Pharmacology Course was developed by a team of nurses who went through nursing school, passed pharmacology, and are/were successful bedside providers. The “nurse” who teaches the course is a pharmacist. It can’t get better than that!
Learning how to rock nursing math can be challenging, but it doesn’t have to be gastric-ulcer-producing. We are going to walk you through some of the important basic concepts to be aware of, as well as some tips and tricks to make things a bit easier.
Keep in mind, that while we will go over quite a bit here, there are a few things that you’ll just simply have to memorize.
PART ONE: 6 Steps to Nursing Med Math Success
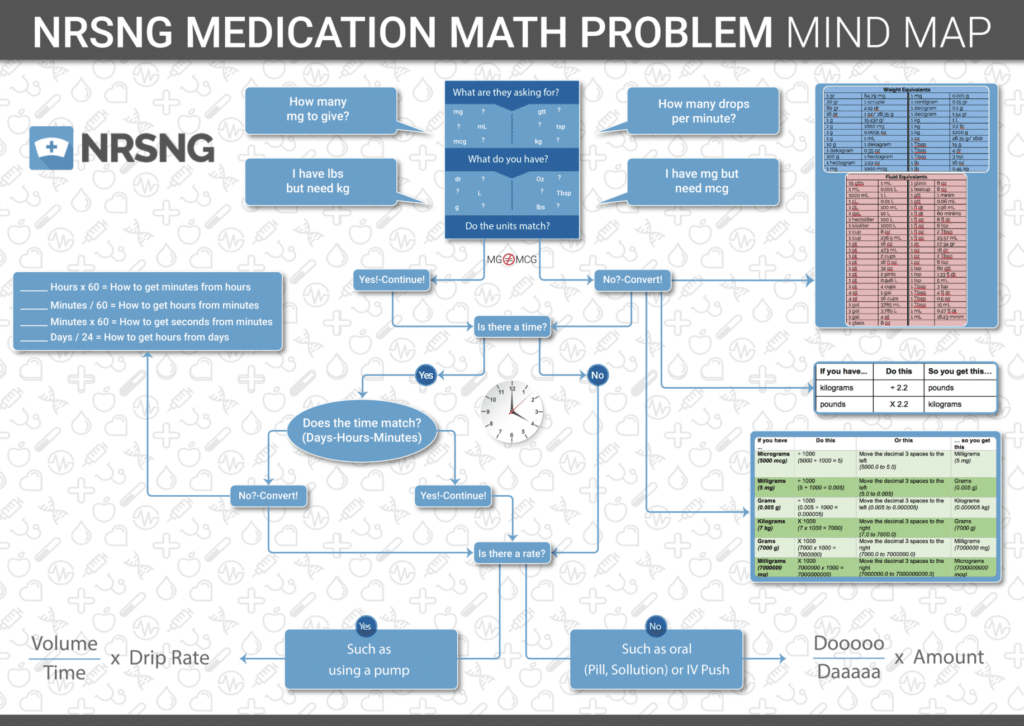
We created an amazing outline/mindmap to help you navigate your math questions! Here’s a quick rundown of our 6 steps to nursing med math success!
- Step 1: What are they asking?
- Step 2: What do you have?
- Step 3: Do they match?
- Step 3A: Convert the units if needed
- Step 4: Is time involved?
- Step 5: Is a rate involved?
- Step 6: Calculate the dosage
We created a mind map to help you navigate through these steps easier, especially if you’re a visual person.
Before I dive into each specific step, I just want to remind you to check out our Med Master course, which is the perfect complement to this post about med math. Understanding the dosage calculations, drip rates, unit conversions, and so forth is one thing, but understanding the pharmacokinetics is another. By understanding both, you will be best equipped to safely administer medications as a registered nurse - or if you want the best nclex prep program, try this.
Alright, now let’s work through each specific step of the NURSING.com Med Math Mind Map. Wow, that was a tongue twister . . .
Onward!
Med Math Step 1: What are they asking?
Nursing math tests are like many of your other exams in nursing school: sometimes there are multiple distractions in the question that you have to weed through to get down to the meat of it. It is important to keep your mind focused on specifically what is asked and what unit you are being asked to answer in.
The question may say something like…
Your patient has 2.5 grams of Vancomycin in 500 ml normal saline to be administered IVPB over three hours ordered, how many milligrams total will this patient receive?
So what are they asking for in this question? They are asking for how many milligrams the patient will receive. We don’t care about the 3 hours, the IVPB, the normal saline, or even the name of the drug! The question is essentially asking you to convert 2.5 g to milligrams.
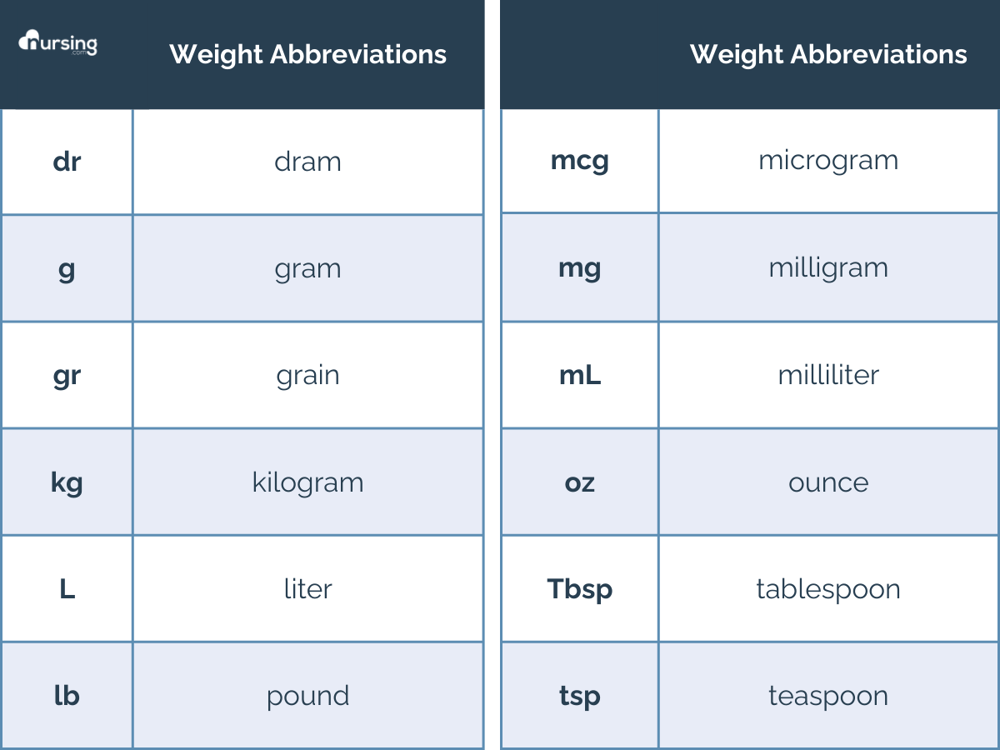
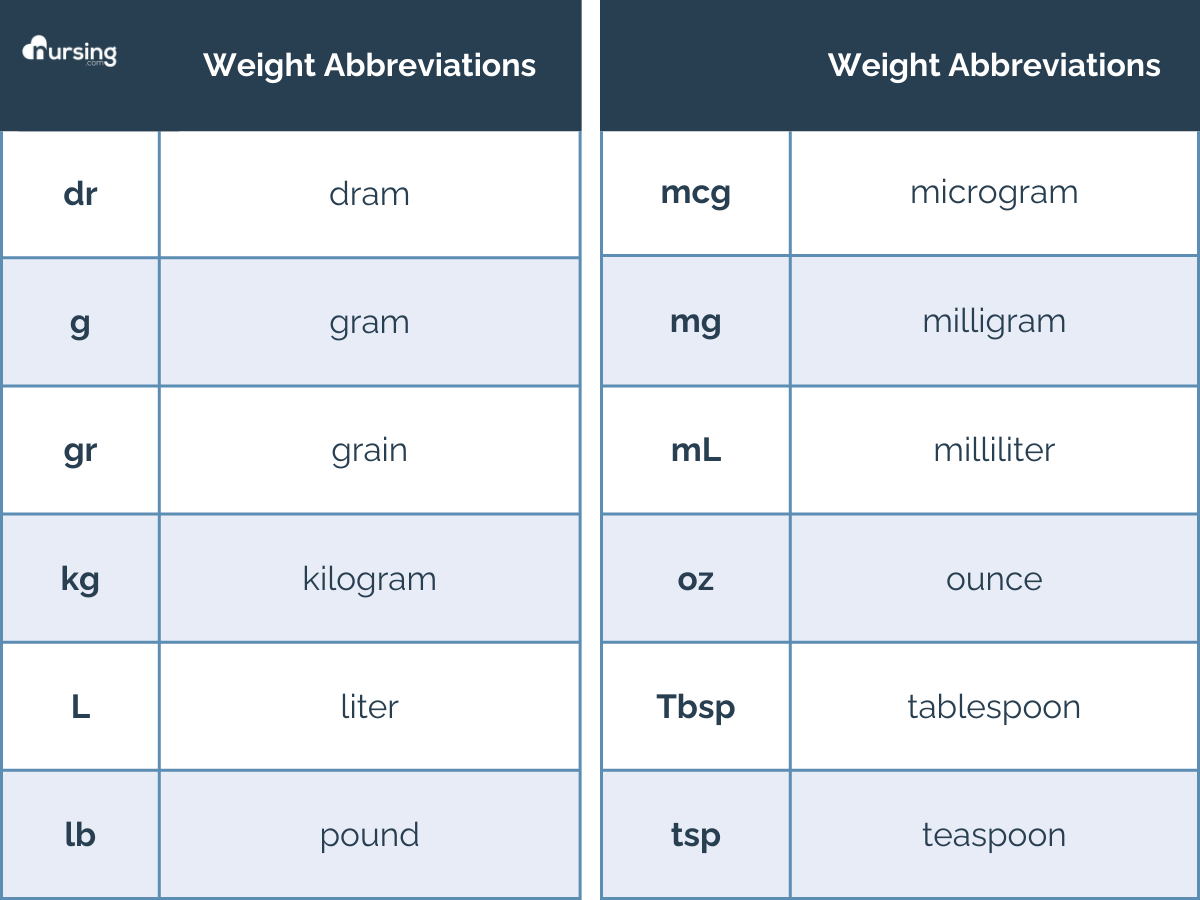
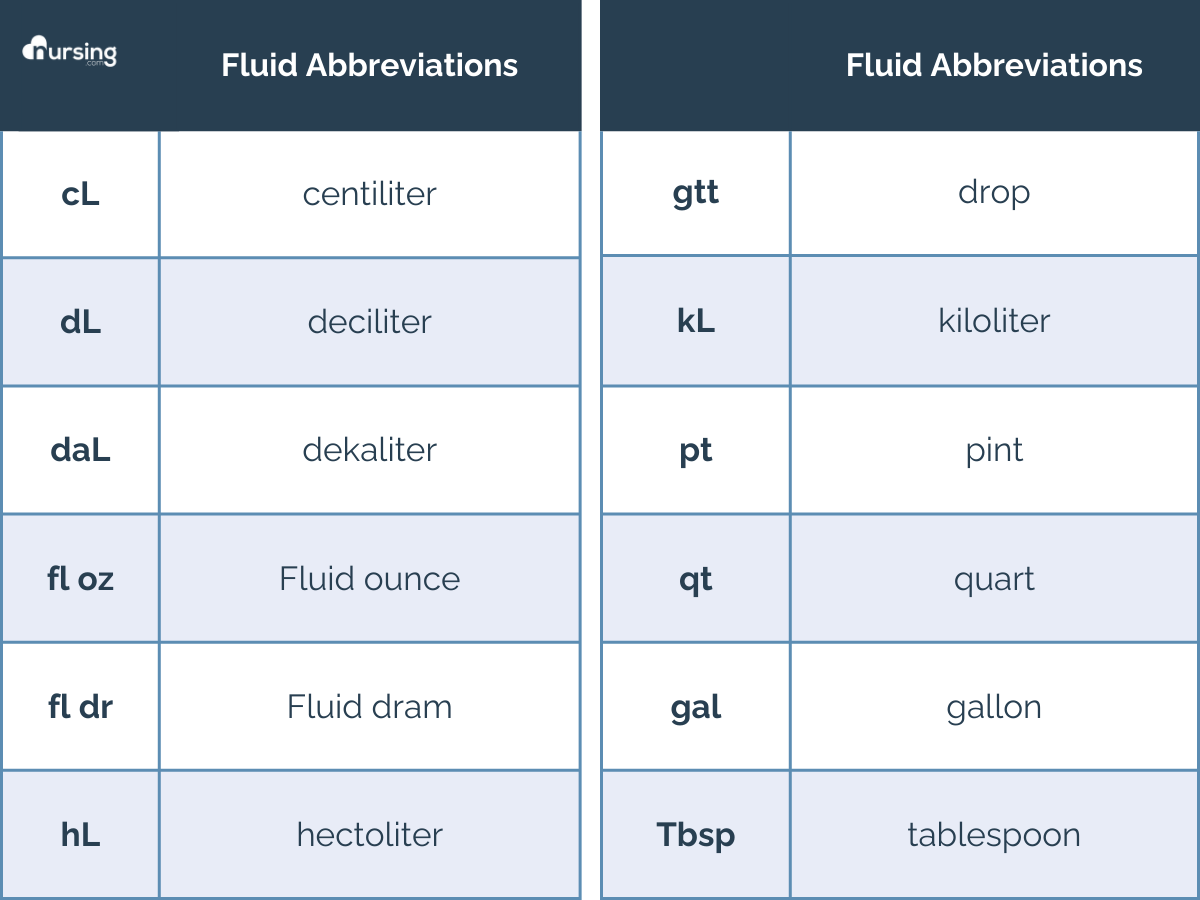
Below is a table of different abbreviations so you can identify various units of measurement. Later, we’ll discuss converting units more specifically. However, for now… it is important to specify what they’re asking for.
Med Math Step 2: What do you have?
What unit of measurement are you working with? Milliliters, kilograms, grams, liters, micrograms?
Ok, thinking back to our Vancomyicin… they told us that the patient has 2.5 grams ordered… but they’re asking for milligrams.
If they match, you’re good. Head on to that next step…
If they don’t, hang on a second… we’ve got to make it so our units match.
Thinking back to our original example… we need to convert grams to milligrams to get the correct answer. We don’t need to worry about the normal saline, the IVPB, or the 3 hours again… the question is merely asking how many milligrams are in 2.5 grams.
Step 3A: Unit Conversion
Okay now that you’re familiar with the specific units, let’s talk about converting them. You may have an order to administer medication in milligrams, but the tablets are in grams. Or you may have a patient who weighs 178 lbs but needs propofol started STAT, which is given in mcg/kg/min. And this isn’t just stuff that you learn in school and never deal with again, you truly need to know this. I promise you, it is valuable.
Let’s go through some basic (you really really need to know this) conversion stuff.
Dosage by Weight
Dosing by weight is something you’ll do frequently. And if you work in pediatrics or with little babies… you’ll be doing this so much that you’ll be able to do this in your SLEEP.
The first thing to know about dosing by weight is that it is almost always done in kilograms. Those of us working in the United States are used to weighing people in pounds, however, it is essential to convert this number to kilograms. Many computerized charting systems will auto-calculate this as soon as you enter the pounds into the chart, however, you must know how to do this on your own.
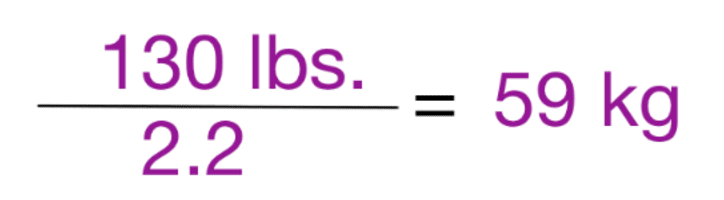
Pounds and kilograms – There are 2.2 pounds in every kilogram.
2.2 lbs = 1 kg
Burn this into your brain.
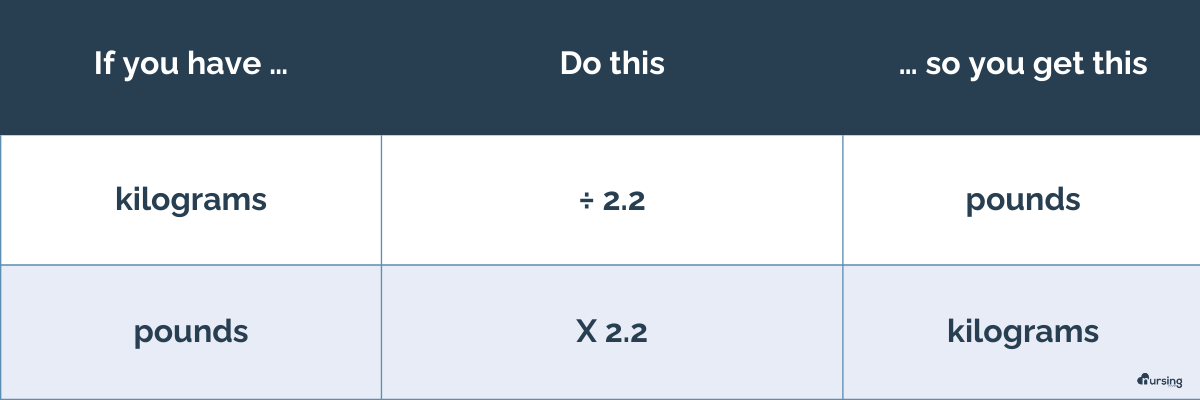
Therefore, when looking at these dosing problems, convert your pounds to kilograms first! After this, it’s a pretty straightforward calculation. You multiply your kilograms by the dose to get the answer.
Example 1 …
Your patient weighs 25 lbs. How many mg will you give your patient if they require 2 mg/kg of medication?
- Let’s change our lbs to kg… 25 ÷ 2.2 = 11.36 kg
- 2 mg x 11.36 kg = 22.72 mg
Example 2 …
Your patient weighs 50 kg. They are on a heparin drip and their PTT was subtherapeutic. The protocol says to give them a bolus of 40 units/kg of heparin. How many units of heparin will you give your patient?
- 50 kg x 40 units = 2000 units
Example 3 …
Your patient weighs 19 lbs. The doctor has ordered a 2 mg/kg of medication, which comes in a 100 mg/2 ml vial. How many milliliters will you give?
- Let’s first convert our weight… 19 lbs ÷ 2.2 = 8.636363.. We will round up to 8.64 kg
- 2 mg x 8.64 kg = 17.28 mg dose ordered
- Now it’s just a simple “dooooo daaaaaaa times amount” question!
- (17.28 ÷ 100 mg) x 2 = 0.3456 ml
- We will round up our final answer of 0.35 ml
So micrograms are the smallest, kilograms are the biggest… and each is a thousand times smaller or bigger. See my handy-dandy chart below. Basically, to go from micrograms to milligrams, you multiply by 1000. To go from kilograms to grams, you divide by 1000. You’re basically moving your decimal point by 3 places to the left or right, depending on if you need a smaller or larger number.
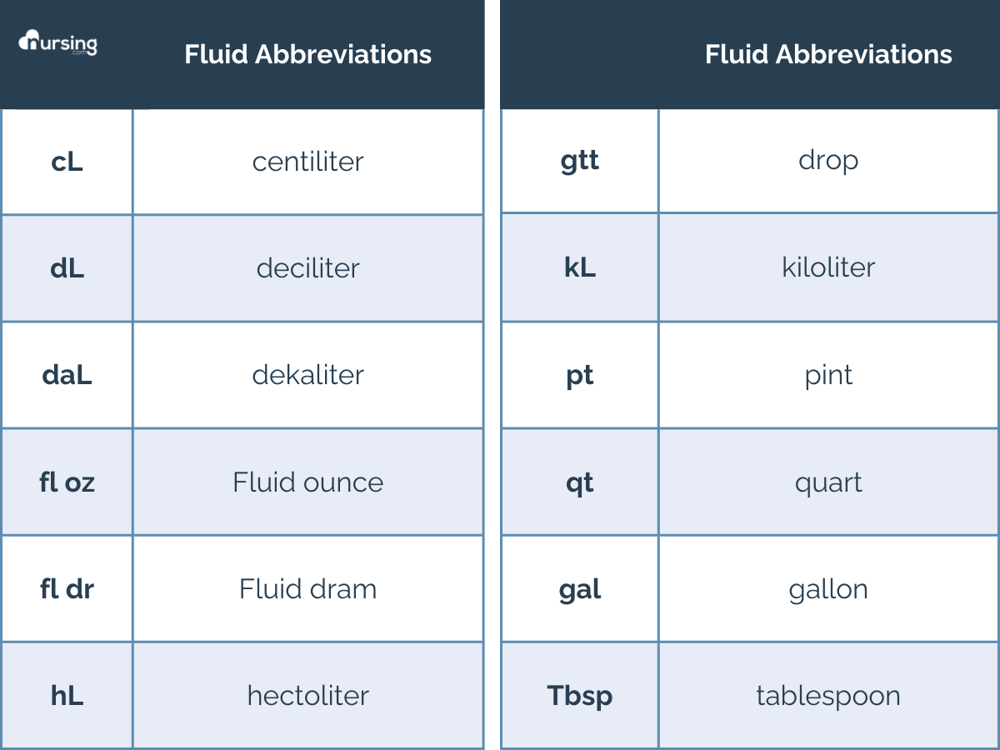
Micrograms, milligrams, grams, and kilograms all measure mass. However, it’s also important to know how to measure volume as well. Use the same principles to convert microliters, milliliters, liters, and kiloliters.
It’ll be important to know that for school, but when you start on the nursing units… realistically, you’ll most likely be working with liters and milliliters. And if you’re working in the neonatal intensive care unit, you’ll start to see those microliters.
.png?width=1200&height=900&name=nursing%20med%20math%20(1).png)
Med Math Step 4: Is time involved?
It’s important to note if time is involved because the unit of time we’re working with must match. So if we’re talking about drops per minute, milliliters per hour, and so forth.
Always remember:
- 24 hours = 1 day
- 1 hour = 60 minutes
- 60 minutes = 1 hour
- 45 minutes = 0.75 hours
- 30 minutes = 0.5 hours
- 15 minutes = 0.25 minutes
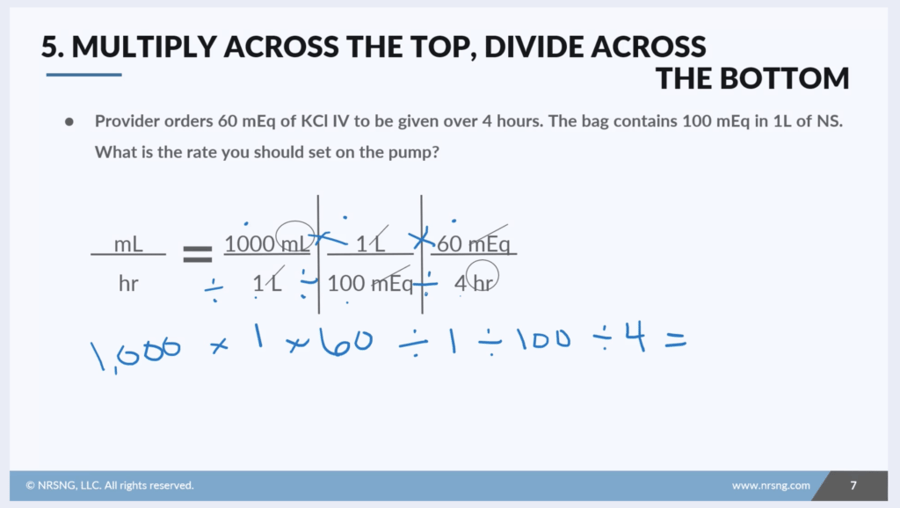
Med Math Step 5: Is a rate involved?
Is this question asking for a drip rate or a pump rate?
Pump rates refer to what you’ll set your IV pump to… whether it be 50 ml/hr, 25 ml/hr, 600 ml/hr, or 83.3 ml/hr.
Drip rates refer to the number of drops at which the IV fluid is dripping at. Basically, the drip rate reflects the number of drops per minute. You can’t measure a partial drop, so rounding is important with drip rates. Make sure you understand the rules your nursing school has about rounding so you make sure to answer the question appropriately.
IV Pumps Rates
This can be tricky, but I promise… it’s doable. In the real world, your IV meds that need to be given via a pump will typically either tell you the rate to plug in, or they will be ordered to be administered over a certain duration of time (for example, infuse over 3 hours, infuse over 30 minutes, infuse over 6 hours) and many pumps today will enable you to enter the duration and auto calculate the rate.
Honestly, in my humble opinion… I truly believe it is safest if the ordering provider orders the medication to be given over a certain amount of time, and we as the administering nurse merely plug in exactly that time, and the pump calculates your rate.
However, we must at least know how to do this otherwise in the event that we work somewhere that does not have pumps capable of this, or if there is a disaster or issue where you need to infuse by gravity… then the whole drop factor/drip-rate situation comes into play.
Keep in mind… the actual probability of that occurring is small, depending on where you work. However, it doesn’t hurt to at least have a basic understanding of how one would go about calculating a drip-rate. But I digress…
You are most likely going to administer an IV medication on a pump, in milliliters per hour, or ml/hr. Figuring this out is pretty straightforward. You take the total milliliters in the dose to be administered and you divide it over the number of hours you want it to infuse over. Remember, it is milliliters per hour. If you can just remember that and repeat that to yourself in your head, it almost tells you the calculation for you. How many milliliters will I infuse every single hour?
This is pretty straightforward, except the only part that can be somewhat tricky is if you need to give the medication over less than an hour.
If you need to give an IV in less than an hour, you need to figure out what fraction of an hour they’re asking you to give the medication over… is it 15 minutes, 30 minutes, or 45 minutes? 15 minutes is ¼ of an hour, so 0.25. 30 minutes is ½ of an hour, so 0.50, and 45 minutes is 0.75. Keep that in mind if you’re asked to figure out the rate of something administered over less than 1 hour.
Remember, you’re administering this in milliliters per hour, so we have to have our time in hours!
Example 1:
- Administer 500 ml over 2 hours. What’s the rate?
- 500 ml ÷ 2 hours = 250 ml/hr
Example 2:
- Administer 50 ml over 30 minutes. What’s the rate?
- 50 ml ÷ 0.5 hours = 100 ml/hr
Example 3:
- 750 ml over 6 hours. What’s the rate?
- 750 ml ÷ 6 hours = 125 ml/hr
Drip Rates
Full disclosure, guys… the NRNSG team never, ever uses this in practice. Like, none of us. We actually had to look up this because we all learned it in school, but never actually used it in practice. That will probably make you feel better or worse… who knows? Some nurses who work out in the field or in very specific areas and specific situations may use this… and there’s always planning for the absolute worst (power goes out, all backup generators go out, all batteries die, a massive influx of 9 million patients and unable to use pumps for everyone…)
Also, keep in mind that rounding is important when calculating these drip rates because you can’t give a fraction of a drop. Your instructor should have specifications for how this will be done for your exams (up, down, what to round it to).
First, you must know the kind of tubing you’re dealing with so you know the drop rate. How many drips per milliliter are we talking about here? 15 gtts/ml? 20 gtt/ml? 30 gtt/ml? This information should be given to you in the question..
Next, you take your volume (in milliliters) and divide it by the time (in minutes).
Finally, you’ll take that number and multiply it by that drop factor you were given (gtt/ml).
[ Volume (ml) ÷ time (min) ] x drop factor (gtt/min) = _______ gtt/min
Example 1:
You need to give 1000 ml of normal saline over 4 hours. The drop rate of your infusion set is 20 gtt/min. What’s the drip rate?
- Let’s change our hours to minutes… 4 x 60 = 240 minutes
- (1000 ml ÷ 240 minutes) x 20 gtt/min = 83.3333…
- Let’s round down for our final answer to be 83 gtt/min
Example 2:
You need to infuse 50 ml of an antibiotic over 1 hour. The drop rate of your infusion set is 15 gtt/min. What’s your drip rate?
- Let’s change our hours to minutes… 1 x 60 = 60 minutes
- (50 ml ÷ 60 minutes) x 15 gtt/min = 12.499999…
- Let’s round down for our final answer to be 12 gtt/min
Example 3:
You need to infuse 500 ml of Vancomycin over 3 hours. The drop rate of your infusion rate is 20 gtt/min.
- Let’s change our hours to minutes… 3 x 60 = 180 minutes
- (500 ml ÷ 180 min) x 20 = 55.55554
- Let’s round-up for our final answer to be 56 gtt/min
Med Math Step 6: Calculate the dosage - Dimensional Analysis Nursing
If you don’t have an IV pump rate or drip rate to worry about, you’re basically going to calculate the dose. With most medications, you’ll give one tab, one syringe full, or something similar. Many things are pre-drawn up in one-time-use packaging to reduce the potential for med errors.
I use this method all the time as a nurse. However, there are some that will require you to give a partial dose. Use this method to determine specifically how much to give. This is necessary because the dose that the patient needs may not always match exactly how it comes. Maybe they need 2 tabs, 6 tabs, 1.75 tabs, or maybe it comes in a 5 ml syringe and they need 2.5 ml, 1 ml, or 10 ml.
Many times, the computer and/or pharmacy will auto-calculate this, but I always double-check this on my phone calculator before administering it. If it’s a high-alert medication or something I don’t routinely give, I’ll double-check my math with a coworker or two. Calculators can also be in the MAR or on the computer you are using if the clinical instructor freaks about having cell phones (mine did).
This quick method was taught to me by a friend.
“Dooooo. Daaaaaa. Times amount.”
Say it again with me.
“Doooooo. Daaaaaaaa. Times amount.”
(Dose ordered ÷ dose available) x amount
So you take whatever dose the physician ordered, divide it by whatever you have available, and multiply that times the amount that the med comes in.
Example 1:
The physician has ordered 2.5 grams and the medication comes in 500 mg/tab. How many tabs will you give?
2.5 grams = 2500 mg
(2500 ÷ 500) x 1 = 5 tablets
Example 2:
The nurse practitioner ordered 50 mg and the medication comes in syringes that are 1000 mg in 4 ml. How many ml will you administer?
(50 mg ÷ 1000) x 4 = 0.2 ml
Example 3:
The PA ordered 100 units and the medication comes in 20 units/ml. How many milliliters will you administer?
(100 ÷ 20) x 1 = 5 ml
PART TWO: Dosage Calculations for Nursing Students (an intro to dimensional analysis)
Let’s get one thing very clear…
The hardest part of figuring out med math problems is making sure the units are correct.
The rest is filling in the blanks in the equation and solving.
So let’s begin with a few reference points.
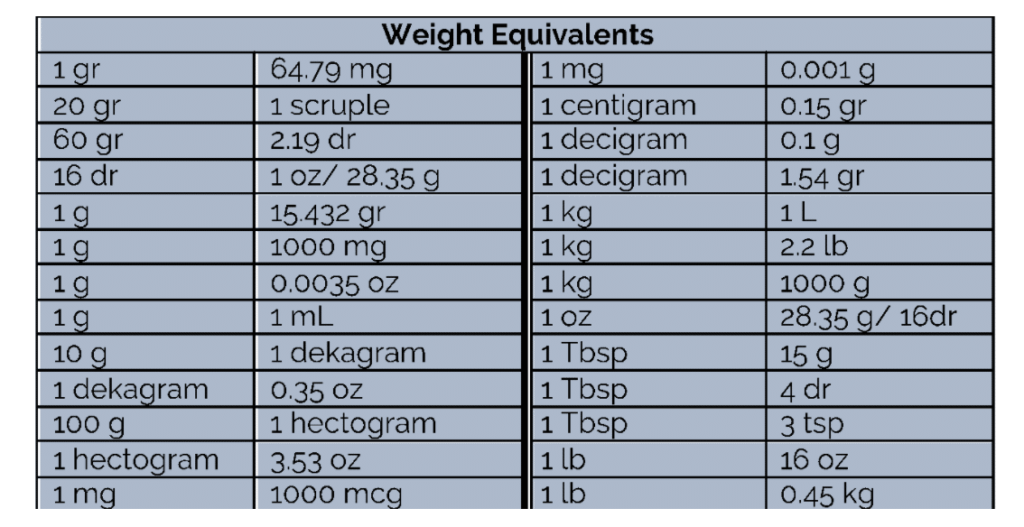
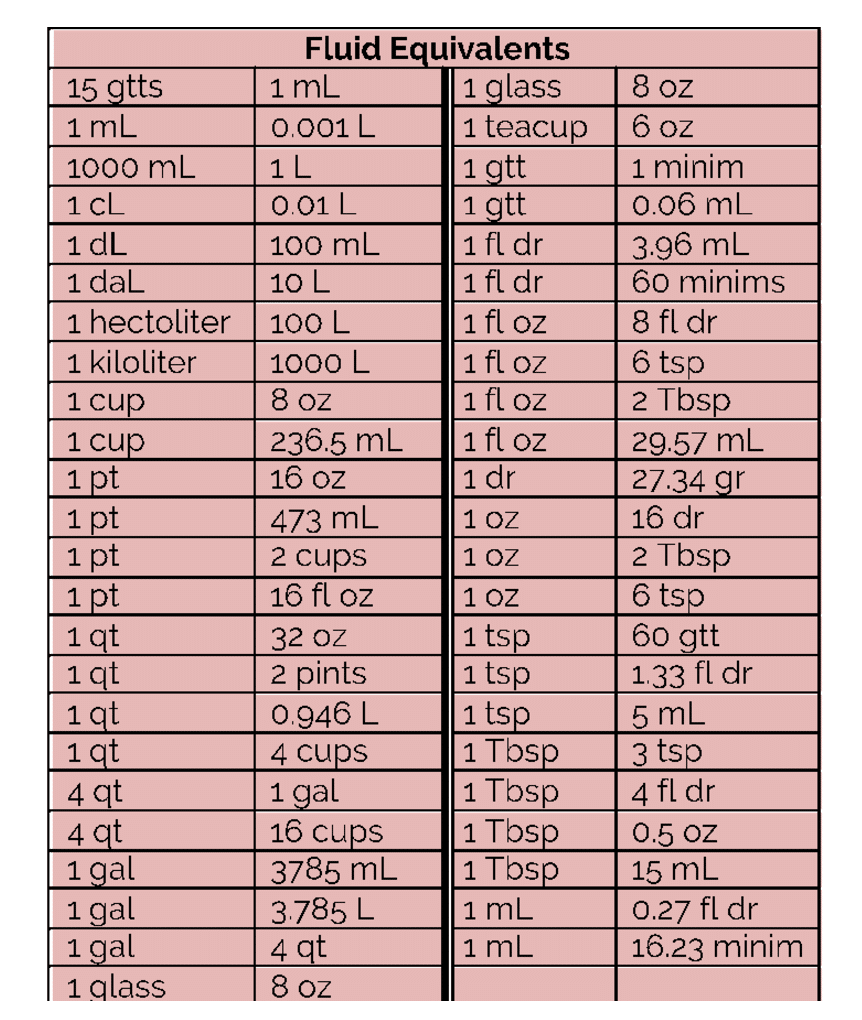
First, what are all these abbreviations and what do they stand for?
Second, what are the equivalents for these units?
So now that you have a reference point let’s talk about figuring out dosage calculations.
There are a few different types of formulas you will need to know.
- Amount in the IV fluid
- Concentration x volume (mL’s)
- Rate of a volume – mL and drop
- Volume/Time
- Volume/Time x drop factor
- Rate of a mass- mL
- Mass/On hand x Volume
- Fluid maintenance
- 0-10 kg = 100 mL/ kg
- 10-20 kg = 1,000 mL +50 mL/ kg
- 20-70 kg = 1.500 mL + 20 mL/ kg
- 70+ kg = 2,500 mL
- Fluid replacement
- 20 mL per kg
- Weight-based
- Lbs / 2.2 = kg
- Kg x 2.2 = lbs
- Weight x dosage per weight
Using the references above, let’s solve some problems.
You are the nurse for a 45-year-old patient who is NPO and needs to have fluids. The doctor orders N.S. at 25 mL/kg per day. The patient weighs 130 pounds. How many drips per minute will the nurse set the macro tubing to?
There are really four parts to this question.
- Converting weight
- Calculating volume in a day
- Converting mL per day into minutes
- Calculating drips per minute
First things first. Get those pounds into kg…
Second, multiply out the mL per kg…
Next, divide the mLs for a day into mLs per minute…
Finally, convert mLs into drips (using macro drip tubing is 15 gtt per mL)…

You can do this!
Take your time, get it right. Read the question carefully and make sure that you are converting things that need to be converted (ie. lbs to kg or hours to minutes). The key to getting good at med math calculations is PRACTICE! Just get as many practice problems as you can and work through them! Good luck! You can do this!
Lastly . . . I’m Bad at Math, Can I Still be a Nurse?
The good news is that you don’t have to be a mathematician to be a successful nurse. You don’t need to master calculus, physics, or geometry… just some basic knowledge that will get you to where you need to be to administer medications safely.
If you are concerned about how you will do on the math portion of the NCLEX - you might want to download our free NCLEX study notes pdf - NCLEX Flash Notes.
And don’t forget – there is no shame in checking your work, no matter how basic it is. I remember when I first started in my critical care unit, I was double-checking a simple math question with a very experienced coworker. She had been a neuro ICU nurse for decades… and when I asked her a math question, she paused and got her phone out and her calculator and double-checked a math question that one could easily do in their head, right on her phone.
It made me feel better to know that wonderful, experienced nurses double-check even some of the most basic math calculations on their calculators with no shame. We truly have the lives of others in our hands, so if you need to double-check an obvious partial dose on your calculator, do it!
Ask your coworkers, talk to the pharmacist, and use your resources if you’re ever in doubt. Remember, it really helps to have as much understanding of pharmacology and med math under your belt as possible.
9 Common Cardiac Medication Classes
Nine common classes of cardiac meds, that you’re going to need to understand, and you’re going to need to know at a very high level.
I hope this post was helpful to you. I know before I said there can be bad news bears with med math, but there’s also a good news bear. And he’s wayyyy cooler.
Listen below as we discuss, on a very upper level, what’s going on, why we give these meds, and really what you need to know about them.
NURSING PHARMACOLOGY STUDY GUIDE