How to Prioritize Nursing Tasks | NURSING.com Blog
Nursing has many components involved. That is why time management in nursing is crucial. It is literally the glue that holds the skills we have learned to become a nurse together. You need to be good at such a large array of things that it can become overwhelming at times.
After you receive report on your patients, you will be building your to-do list.
They key to managing the to-do list is to have a clear hierarchy of tasks that can be flexible as things change and to be comfortable with delegation in nursing.
Start with the ABCs
- Airway
- Is the airway patent?
- Breathing
- Rate, depth, pattern and sounds of breathing
- Circulation
- Heart rate, BP, perfusion, beating of the heart (What is their EKG?)
This is actually the easiest part of prioritizing. You will need to adjust any plan you put into motion if an ABC becomes compromised.
As for the other tasks, which I will call non-urgent tasks, you can plan these tasks to make your day go more smoothly and efficiently.

Non-Urgent Prioritization
So everyone’s urgent needs are taken care of. There are just non-urgent tasks to complete. Check out our post on stable patient prioritization.
You can separate the tasks into categories that help you decide what to do first. I generally separate them into the following categories:
- Things that require action before they can happen
- Things that are time sensitive
- Things that other people can do
- Patient schedules/appointments
- How many items a patient needs to have done
Then I try to get a timeline together of when certain things must be accomplished and work from there, filling in the gaps and grouping activities if possible.
Tips to working smarter, not harder
A key thing to think about when prioritizing in nursing is how to get the most amount of things done in the safest and most efficient way. Usually, this requires you to work smarter, not harder. I mean when I say this to combine tasks if possible, anticipate certain tasks, set yourself up for success.
For example, there are a few tasks that I do on almost every patient, and then there are tasks that I do every time per patient complaint or need.
Almost every patient will:
- Get hooked up to the monitor (if available) for continuous vital signs.
- Give a urine sample if they go to the bathroom.
- Side note: If your patient will need a urine sample because they are complaining of burning upon urination let say, then it is helpful to have that be the first thing you do with that patient. Go into the room and before hooking them up to the monitor, take them to the bathroom and get that urine sample.
- Get an update of what is next before you leave the room. (Trust me, this will save you time in the long run)
Specific patients needs:
- If getting an IV:
- Draw the rainbow (all the tubes) and hold them.
- If they need blood work:
- Put in an IV so you can potentially draw more blood if needed, or give medication if needed. (It saves the patient pokes)
- If they complain of Chest Pain/Shortness of Breath:
- Get an EKG, start an IV, draw blood, and place them on the monitor.
- If they are febrile or have a suspected source of infection (cellulitis for example):
- Draw a set of blood cultures and hold them just in case.
Imagine that the patient really has to use the bathroom so you take them to the bathroom and then get them hooked back up to the monitor, warm blankets applied and lights dimmed. All of a sudden the doctor orders a urinalysis… If you had just gotten that a few minutes ago when the patient was going you wouldn’t have to wait to get it, have this looming task over your head that might be awhile before you can accomplish it.
Or let’s imagine a scenario where your patient says they are in 10/10 pain and you ask the doctor for pain medication and the doctor asks you for the last BP… if you had the patient hooked up to the monitor you would have a recent BP.
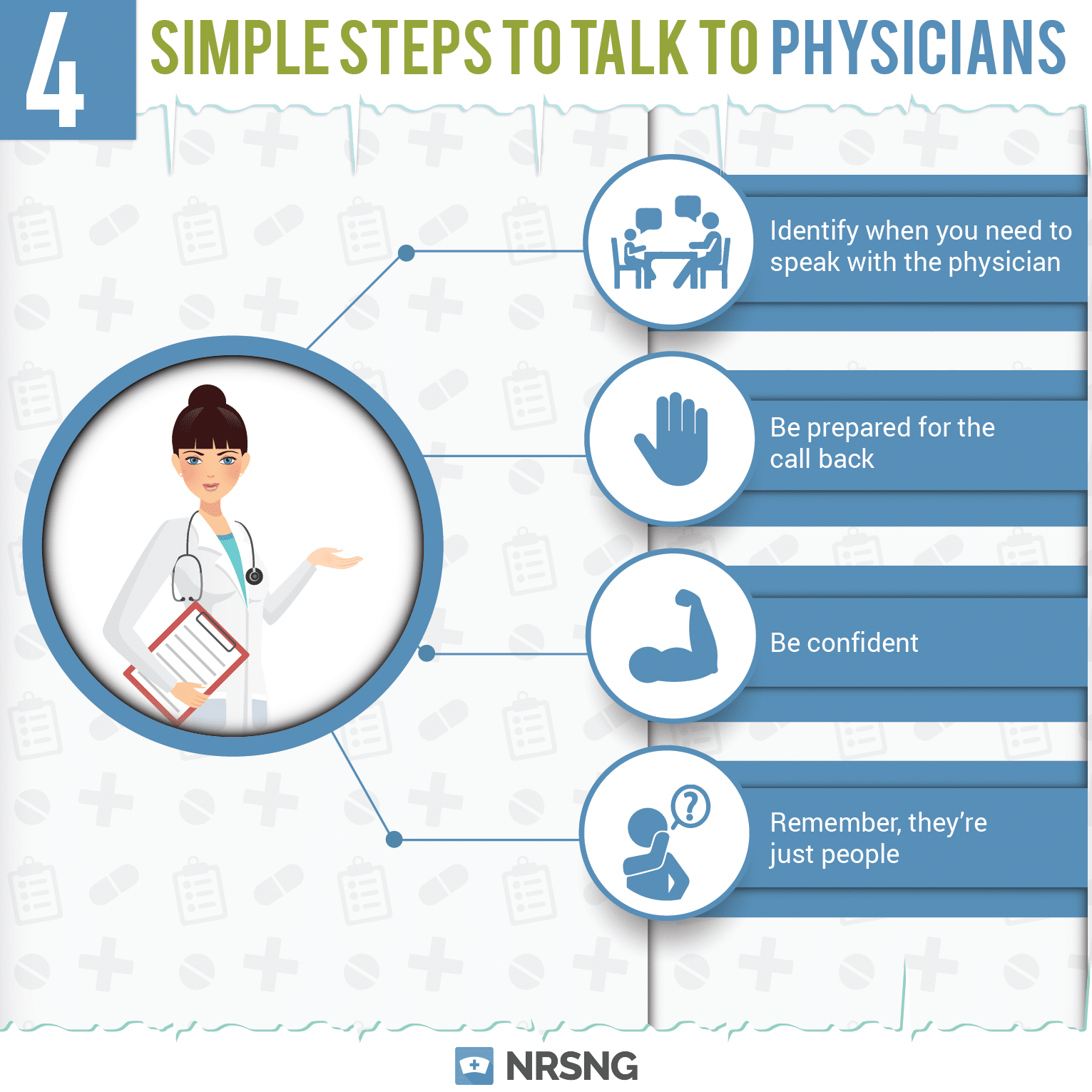
Speaking of talking to the doctor….
Before you talk to an MD

Before running to the doctor, save yourself some steps by gathering some information first:
- If a vital sign is abnormal:
- LOOK at the patient- symptomatic or not?
- Double check it: do it manually
- Check trending vitals
- If the patient needs a medication:
- Check the chart, is it ordered?
- What was the last set of vitals?
- What are the patient’s allergies?
- Have they ever had the medication before?
- If it is a home med, is the medication in the chart correct? (Use the 5 rights of medication administration)
- If it is a pain medication, when was the last dose? What is their pain score?
- If there is a change in patient condition:
- Does the change involve the ABCs?-If so, assess for life threatening issues and call for help. Have someone else get the doctor, do not leave the patient.
- If patient is stable:
- Get a full set of vitals
- Check to make sure there aren’t orders in for you to address the situation
- Ex: patient has a fever and Tylenol is ordered PRN for fever.
- Check to make sure there are nursing protocols you can initiate without a doctor.
- Get lab results (most current and trending)
- Assess the patient for symptoms
- Ex: Patient has a low HR-Are they dizzy-do they feel SOB?
- I cannot stress this enough: LOOK AT THE PATIENT!-Do not treat numbers for the love of god. If their BP is too low…think: are they symptomatic?-do they usually have low BP?- Have you double checked it?- Have you checked manually?

Delegation in Nursing
This can be a tough thing for people to do effectively. Just because there are tasks that can be delegated, does not mean it should be delegated. At the same time, just because you can do everything doesn’t make it efficient for you to do so.
When choosing to delegate, think about the following:
- Is this something you could do while in the patient’s room?
- If yes, don’t delegate
- Is this task time sensitive?
- If yes, delegate
- Is the person you are asking busy?
- If yes, don’t delegate
- Is the person qualified to do the task?
- If yes, delegate
When planning out the tasks that need to be covered, try to consider these time saving tips. They will help you be more efficient and make sure that everything that needs to get done, gets done. For more tips on how to manage your time in nursing check out Everything You Need to Know About Nursing Time Management
How to Prioritize When Everything is Urgent
It can be overwhelming when you have a list of things to do and everything needs to be done right now. Creating nursing diagnoses can be that much more complex. The hope is that you will have help, the reality is that you probably won’t have help and you need to decide what to do first. Or you are taking the NCLEX and you need to answer the question on prioritization correctly.
No matter the reason, nurses choose daily which task is going to be done first. It can be hard. I have to do it daily in the ER when I tell someone their emergency isn’t as emergent as someone else’s emergency and that is why I am taking someone else before them.
So how do you make those decision?
You start with the basics. That’s right, go back to the ABC’s.
Airway, Breathing, Circulation
Don’t get stuck on the order, use the order (A then B then C) to determine if you have two very serious situations and HAVE to choose one to attend to.
Here is an example: you have two patients, one with weak thready pulses and one in respiratory distress. Who do you see first? Respiratory distress. But you can’t just use the ABC’s because if someone is bleeding out and someone has a cough, you see the bleeding patient, so how do you differentiate which ABC is the urgent one?
Supplement the ABC’s with vital signs.
Abnormal Vital Signs
Try to not be concerned about slightly abnormal vital signs (i.e. respirations of 21) if you are not using other pieces to the puzzle. And don’t use vital signs by themselves, you need to pair it with an abnormal ABC.
You have two patients with an asthma attack. One is breathing 40 times a minute with a pulse oximetry reading of 93%. The other is breathing 30 times a minute with a pulse oximetry reading of 84%. Who do you see first? The patient with 84% oxygen saturation because hypoxia is detrimental to the body’s cells, specifically the brain. They both are urgent and need to be seen quickly but if you can only see one, hypoxia is the most urgent.
For more information on SpO2 . For more on the difference between CPAP and BiPAP
The next thing you need to consider is age.
Very Young and Very Old

The very young and the very old are more urgent than everyone else because they are immunocompromised. A 5-day old with a temperature of 101F is more concerning than a 25-year-old with a temperature of 103F.
Conclusion
This takes practice. You will second guess yourself, and it won’t come as naturally to you as it does to an experienced nurse, but having the right foundation can really make the difference.
When reading your text books, try to ask yourself, “Is there a situation where this particular patient with this particular disease process or condition becomes concerning?” For example, when you are reading about the respiratory system and come across the section on asthma, ask yourself, “What is the most concerning situation someone with asthma could be in?” Answer: hypoxia secondary to closed airway.
I hope this helps, and remember using the ABC’s, vitals, and age can help you build a foundation for prioritizing patients and/or tasks.
Be That Nurse . . . (your patients may forget your name)
I Love You . . .
My first shift in the Neuro ICU all by myself as a new nurse I was assigned a patient who was scheduled to withdraw life support during my shift.
The family gathered. The ventilator was turned off. And within 30 minutes the patients heart stopped beating.
My job became caring for the family, helping them cope, and educating them on the procedures that would follow.
As the patients mom said goodbye to her son for the last time, she stopped before leaving the unit and gave me a big hug and said to me:
“I love you, I will never forget you. . . ”
She Was Done Fighting
Not more than a week after that experience I was assigned a young 40 year old mother of 3 sons who had been battling cancer for 5 years unsuccessfully.
I had taken care of this beautiful woman on many occasions as she was frequently in our unit. During this hospitalization it was obvious that she was done fighting.
The BiPAP was no longer able to provide her the support she required and she had decided not to be intubated again.
About halfway through the shift, with her husband and children gathered at her side, she took off the BiPAP and passed away.
It was impossible to hold in the tears as I spoke with her young sons. We talked at her bedside for a few hours and shared tears and laughs before they kissed their mom/wife goodbye.
As they left, they thanked me for taking care of their mom.
Patients and families will ALWAYS remember their nurse.
Bring Light to Your Patients
The nurse that brings a light during the darkest time of their life.
They will forget their doctor, they will eventually forget the pain . . .
but they will NEVER forget that nurse that sheds a tear with them, that holds their hand through the night.
At NRSNG . . . our goal is to hold YOUR hand in your journey to RN.
Nursing is a team sport . . . we’ve been where you are now and NRSNG.com is our way to give back.
Be that Nurse!
The WORST Shift of My Life (it’s time to fix patient ratios)
The Registered Nurse Safe Staffing Act will hold hospitals accountable for development and implementation of unit-by-unit staffing plans.
Requires:
- Establishment of staffing system to ensure appropriate # of RNs staffed
- Public reporting of staffing information
This is important because there are no standards by which hospitals set staffing ratios. There are recommendations, but no one is being held to them.
How to Get Involved
Join the Facebook event page: National Rally for Nurse to Patient Ratios
Visit this page to read more about the event: SMYSofficial.com
Coping with the Death of a Patient and Post Mortem Care
Any tips on coping with your first time doing postmortem care? mine was in the NICU.
Death is a difficult reality of nursing care. This episode discusses post-mortem care and coping strategies for nurses when a patient passes away.
"When a patient dies you become a nurse to the family."
Podcast Transcription
The podcast today is going to be a little bit shorter. It’s just going to be me giving some stories and some tips. Because we had a question last night on Facebook, and it was one that we don’t get very often. It was one that I didn’t have any resources available for. The question came from a nursing student who asked, “Any tips on coping with your first time doing post-mortem care? Mine was in the NICU.”
Now, I had to stop and think about my experience with post-mortem care. I remember the first time I did it was actually as a nursing student. I was on a respiratory floor, and it was the step down unit for the ICU. There were a lot of patients that actual had conditions that were very difficult to deal with. I remember I showed up one morning for my rotation as a nursing student, and the off going shift, the night shift, was preparing a body to take down to the morgue. This was my first time do post-mortem care, so we had to identify the body. We had to prepare the body. We had to place the body in the body bag, and we had to take the body down to the morgue, and do all of what’s involved with that. At the time it was very strange to me because I wanted to take good care of this body. I wanted to show respect.
After nursing school I got a job in a neuro ICU, and in the neuro ICU you see death very often. It’s something that if there’s not a death during your shift it’s going to be your next shift. Not necessarily with your patient, but it just happens a lot. It was a very big ICU, 34 beds. All neuro patients. With neuro patients a lot of the condition you see, you might see aneurysm ruptures, you might see sudden strokes, and you might see patients that come in who weren’t aware, but had a very aggressive cancer growing in their brain. They’ll come in, and they were normal with their family the day before. They come into the neuro ICU, and within 24 hours they pass away, so very abrupt, very devastating, very traumatic. Just terrible deaths that we would see, and it took a lot of adjusting. It took a lot of getting used to. I don’t know that getting used to it is the right word for it, but it took a lot of adjusting to be able to cope with this.
I’m going to tell you some of my suggestions. First of all, it’s okay to feel sad. It’s okay to feel uncomfortable, and it’s okay for it to effect you. We’re nurses. We’re not super human. We have emotions. We have feelings, and when you see death, and when you touch a dead body that might be the very first time you’ve ever done that. It might be the first time you’ve ever seen a dead body. It might be the first time you touched a dead body, and then to prepare a body to take down to the morgue is a very humbling experience. We’ll get into that in just a minute.
What I want to share with you guys are some of the things that I have found can really help make the experience better. The first thing I want to say is the best advice I can give you is to be there for the family. If there’s a family there, if there’s family members, friends there your job as the nurse turns. It’s a very strange adjustment because what will happen is you’re there taking care of the patient, and the patient passes away, and now you really have to revert and change all of your focus to the family. You become the nurse for the family. While you’re taking care of a patient you are there for the family and everything, but you become a nurse for the family, and you be there, and you comfort them, and you instruct them, and you teach them about what’s going to happen with their loved one.
The best thing that you can do is really be there. Be that shoulder for the family. Be that strength for the family, and listen to them, and let them share their stories and their experiences. Try to be as compassionate, and loving, and as understanding as you can be.
There was one patient that really stuck out to me. It was a patient who came in, and the family had decided to withdraw care, and the patient had a pacemaker. With a pacemaker you have to place a very strong battery over the pacemaker in order to deactivate it so that the patient will actually experience cardiac death. When this family all got there, it was a very large family, they were filling up the rooms, filling up the floor corridor. It was a very strange dynamic between the mom of the patient and one of the siblings of the patient because they were trying to decide who was going to make all the decisions about what was going to happen with the body after, and so they were really struggling there. My job really became coordinating that.
As nurses we’re care coordinators, and so I had to make sure I got the chaplain there to help explain everything, and get the phone numbers they needed for funeral homes. I had to be there and make sure that the battery was working, and that the patient was clean for the family. I wanted to be there and show the family that I was with them, I was there, and they could reach out to me if they needed to. When the patient did die, when the heart did stop, we extubated the patient, took all the IV lines out, all the central lines out, and everything so the family could say goodbye. Then we were cleaning the patient, taking care of the patient. Making sure the family could touch them and feel comfortable.
The family stayed there for a couple hours, and as the family was leaving the mom reached over to me and gave me a big hug, and said, “I will never forget you. I love you.” It was just the simple acts of being there with the patient’s family, holding their hand, and showing them that I don’t see their loved one as just a body, as just a number, as just something that I have to take care of for my day to get through. I see them as their loved one. It can be hard to really see that and show the family that you see their loved one as someone that you care about. The best way you can do that is to really just show care for the body, take care of the body, keep the body clean, keep the curtains closed, keep the lights on, ask other people who are not part of those family members to keep it down there’s a death, and those types of things that you can do to really show them that you’re paying your respect to the family member.
The next thing I would really recommend is that you need to find somebody to talk to about this. One thing that I think that really needs to exist in hospitals are debriefings after death. Because what happens is I think we bury the feelings because there’s not real way to express how we feel. It can be hard too because as nurses we do want to be strong, and so it can be hard to say, “This one really affected me.” I think what really can be helpful is if you have a spouse, a loved one, a partner, a friend, a parent, whatever it is. If you have somebody that you can reach out to in these shifts and these experiences that are really hard. Somebody that you can reach out to and talk to.
For me, I always had my wife. She works ICU as well, and so I was able to share with her some of the really hard experiences. When there were shifts that I just didn’t know if I was going to make it through I had her to that I could talk to. I know everybody doesn’t have that person. If you don’t have that person have a journal. Even just talk it out, and record it, or anything that you can do to get the feelings off your chest because what I see happens with some nurses is they develop bad habits trying to deal with all the difficulty of the job. Some bad habits might eating poorly, or sleeping poorly, or alcohol. Find healthy habits. The biggest thing that you can do is find someone that you can talk to.
I remember there was one patient that I had that just really affected me. He had children my age. He was about almost exactly my age by just a couple weeks. He had a little daughter that was 1-year-old, and my daughter was 1-year-old at the time. He came in, and he passed away of a very unknown condition, and just died very quickly. That one really, really touched me. Really, really affected me. I took care of him and the family for three days straight on my full three day shift there. It was a patient that I hugged everyone in the family. I became friends with a lot of family on Facebook. I did my best to really show them that I cared because I was truly, deeply affected by them, and I let them know that.
I said, “Some patients just stick with you forever.” This was a patient that really did stick with me forever. As the shift ended after he passed away, instead of going home that morning I went to my parents’ house. I sat down with my parents and I just told them that I loved them. I told them how precious life really is, and that’s what I really want you to take away from this podcast, and from experience you have with this is that as nurses … I don’t think that dealing with death is necessarily a positive thing. It’s a burden of the job, but you can take positive things out of it. We can live life a little bit sweeter. We can be a little bit happier in life because we get to see how precious it really is.
That morning, as I was driving home it didn’t matter to me if I was being tailgated or tailgating somebody. It didn’t matter to me. The little things in life, my student loans and things like that, I wasn’t worrying about those things. What I was thinking about was my child, my kids, my wife, and my parents, and that’s exactly where I went immediately was just to tell my family that I loved them. We really get experiences in nursing. Those opportunities to see how fragile, how precious, how real life really is, and how quickly it can all be taken from us.
Those are the two things I’m going to tell you. First of all is just find someone you can talk to. Get healthy habits. Lastly, I just want to talk about the process generally of post-mortem care. I’m not going to talk about all the different ways that will lead up to post-mortem care, but I’m going talk to you about some of the things that have to happen when a patient does pass away.
First of all, you have to fill out a lot of paperwork. There’s a lot of paperwork to fill out, and you have to get the physician there to declare death if you’re in a state where nurses can’t declare death. Once death is declared you have to … This is for Texas. I don’t know necessarily for every state, but you have to coordinate a lot of care. One of the people you need to get on board is the chaplain. What the chaplain’s job is, is to really kind of work with the family as you’re trying to take care of all the other pieces of the job. They work with the family on funeral homes, on finding the funeral, on working with them on figuring out who’s going to pick up the body after we take it to the morgue. They let them know when that’s going to happen, and so they really do a huge job in this. They really play a very big role in post-mortem care, so you need to get the chaplain there and let them know that the patient has passed away. At the beginning of a shift, if I have a patient who I think might pass away I’ll get them there.
You need to be coordinating with the physicians so that they can write the death certificate. They need to write the death certificate, and make sure that they write some sort of note in the chart that they were there, they pronounced the patient dead, and that’s the new diagnosis. The other thing you need to do is you have to fill out something for the coroner. You have to let the coroner know if this patient needs to be investigated. Some things that would require that are if they die within 24 hours of coming to the hospital, if they died in restraints, and if there’s any sort of pending investigations from this. It was homicide, or anything like that that might require a coroner investigation. You fill out all this paperwork. You have to call them.
Then as the patient starts to look like they might pass away … This happens a lot in neuro ICU. If it looks like they’re going die from brain death especially, you are going to call donation services. What that is, is that’s like tissue donation. You would call them, let them know you have this patient that’s going to die, and you let them know a lot of information about the patient. Age, diagnosis, lab values, all these types of things, so that they can run in through their database, figure out if this is a patient who would be a candidate for tissue donation. That can take up a lot of your time.
Then what you have to do is you have to really break down their chart, make sure you have all the kind of ducks in a row. That everything’s been charted on this patient everything’s taken care of. Then a big thing that you really have to do, like I said, is really keep the patient clean. Once the patient does die you usually give the family some time. I usually let them know, “You can stay as along as you want.” Usually most people will just leave within a couple hours. You don’t really don’t want families to stay much beyond that because the body will start to become very stiff, blood will start to pool, and things like that. It’s good to really have the family gone within a couple hours. I’ve never really seen families stay longer than two or three hours.
Once the family’s gone you will remove all tubes, all IVs, and everything, unless it’s the coroner case. If it’s coroner case you leave all that in. If it’s not you’ll remove all the IVs. You’ll remove all the Foley’s. You remove all the ET tubes, all the bandages, everything from the patient. Then you really wipe the patient down, clean the patient up, and just kind of make them look clean. Then you will go to the morgue, and you’ll get a gurney and a body bag. Then you’ll bring that up, and you’ll place the patient in a body bag and a clean gown, and you will wheel them down and put them in the morgue. Usually you leave some sort of note so that the chaplain and funeral services know that the body’s in there. That’s kind of the steps.
I know that might sound kind of harsh. That might sound kind of mean, but that’s really what happens when you do all that. Then you’ll come back up to the room, make sure charts all put away, everything’s all put away, and then you let housekeeping and everything know to come clean the room. Then you have a new room and stuff like that. That’s really how that works. That might sound kind of harsh and everything, but that’s really the step by step process of how it works.
The important thing is that you find a healthy way to cope with it. Again, I’ll tell you the best thing you can do is to divert your care to the family, and to really take care of the family, and then after to take care of yourself. Be strong enough to let people know that it affected you. It’s okay for it to affect you, and that doesn’t make you weak. That doesn’t make you a bad nurse. It’s okay to feel those things. It’s okay to not make jokes, or to not say anything crude or anything about these people. That’s really my suggestions, my tips. I know that’s kind of an off the cuff quick podcast, but I wanted to give you guys my take on post-mortem care.
If you guys have any struggles with this be sure to reach out to us. We’re here. If you don’t have anybody else you can talk to let us know. You can reach out to us on social media, or through our e-mail address, or on the website, and we’re here for you guys. We want you succeed. We want you to be confident and comfortable nurses. Anyway, anything you guys need let us know. We’re always here for you. We want to be your biggest champion, and we want you guys to be a part of this.
Thank you so much for being part of the NRSNG family. We love guys. Appreciate everything that you do. You guys know what time it is now. It’s time to go out and be your best self today. Happy nursing.


.png?width=50&height=50&name=image%20(11).png)