NCLEX Exam Review on Congestive Heart Failure + FREE eBook Download!

Understanding Congestive Heart Failure is Crucial for the NCLEX Exam
CHF is a chronic and life-threatening condition affecting many patients worldwide. Being knowledgeable about CHF's pathophysiology, symptoms, risk factors, and management is critical for nursing students, as they will encounter such patients throughout their careers.
On the NCLEX exam, questions related to CHF may assess a nursing student's ability to recognize signs and symptoms, prioritize interventions, and understand the importance of patient education for self-management and treatment adherence.
.png?width=1200&height=630&name=nclex%20review%20for%20angina%20(2).png)
Heart Failure Overview
The heart is a pump, it circulates blood throughout the body. Heart failure = pump failure. Heart failure occurs when the heart cannot pump enough blood to supply the body's needs.
General Information on Heart Failure
- Pump failure → decreased perfusion forwards and increased congestion backward
- Causes
- Myocardial Infarction → dead muscle can't pump
- Hypertension → ↑ afterload = ↑ stress on the heart muscle
- Valve disorders = inefficient pump → blood not moving in the right direction
- Diagnositcs
- BNP (Brain Natriuretic Peptide) → a hormone secreted by cardiomyocytes in response to stretching of the ventricles
- Echocardiogram to detect ejection fraction and can diagnose valve disorder
- Chest x-ray to detect cardiomegaly and pulmonary edema
- Complications
- Volume overload
- Decreased perfusion
Nursing Assessment for Heart Failure
- Right-Sided Heart Failure
- Decreased Pulmonary Perfusion
- ↓ oxygenation
- ↓ activity tolerance
- Decreased Pulmonary Perfusion
- Increased Systemic Congestion
- Blood pressure
- PERIPHERAL EDEMA
- ↑ Jugular Venous Distention (JVD)
- ↑ Preload
- Weight Gain
- Fatigue
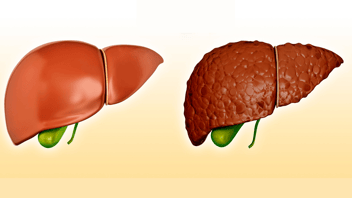
- Liver / GI Congestion
- Blood pressure
- Left-Sided Heart Failure
- Decreased Systemic Perfusion
- Skin pale or dusky
- ↓ PERIPHERAL PULSES
- Slow capillary refill
- ↓ renal perfusion
- ↓ urine output
- Kidney Injury / Failure
- Increased Pulmonary Congestion
- Pulmonary edema
1. COUGH
2. PINK/FROTHY SPUTUM
3. Crackles
4. Wheezes
5. Tachypnea
6. SOB on Exertion - Anxiety/restlessness
- Pulmonary edema
- Decreased Systemic Perfusion
.png?width=1200&height=630&name=nclex%20review%20for%20angina%20(2).png)
Therapeutic Management for Heart Failure
- The goal is to decrease the workload on the heart while still increasing cardiac output.
- Decrease Preload
- Decrease Afterload
- Increase Contractility
Nursing Case Study for Heart Failure
Patient Profile:- Name: Mary Johnson
- Age: 65
- Gender: Female
- Medical History: Hypertension, Type 2 Diabetes, Hyperlipidemia
- Occupation: Retired teacher
Chief Complaint:
Mary presents to the emergency department with complaints of increasing shortness of breath, especially during physical activities like walking up stairs. She also experiences fatigue, frequent nighttime urination, and difficulty lying flat at night due to shortness of breath.
Assessment Findings:
- Vital signs: Blood pressure 160/90 mmHg, Heart rate 95 bpm, Respiratory rate 24 breaths/min, Oxygen saturation 88% on room air, Temperature 98.6°F (37°C).
- Cardiovascular: Jugular venous distention (JVD), bilateral peripheral edema, crackles heard on lung auscultation, S3 heart sound present.
- Respiratory: Increased work of breathing, labored respirations.
- Skin: Pale, cool, and clammy.
- Blood glucose level: 180 mg/dL.
Nursing Interventions:
- Immediate Assessment: Prioritize assessing Mary's airway, breathing, and circulation (ABCs). Administer supplemental oxygen to maintain oxygen saturation above 90%.
- Administer Medications: Administer prescribed medications, including diuretics, ACE inhibitors, and beta-blockers, to manage fluid overload and blood pressure.
- Monitor Fluid Balance: Record intake and output to assess fluid balance and evaluate the effectiveness of diuretic therapy.
Outcome:
Mary's shortness of breath improves with oxygen therapy, and her oxygen saturation increases to 92%. Diuretics help reduce her edema, and her respiratory effort decreases. The healthcare team diagnoses her with congestive heart failure (CHF) exacerbation. Mary is admitted to the cardiac unit for further management, including diuresis and medication optimization.
Conclusion and Free Download
This Heart Failure review has equipped you with essential knowledge for tackling the NCLEX with confidence. Understanding the symptoms, interventions, and considerations related to Heart Failure is vital for providing exceptional patient care as a nurse.
Looking for more must-know NCLEX review topics? Download our free eBook, "NCLEX Flash Notes: 77 Must-Know Nursing Topics for the NCLEX," by simply providing your email address below. I'll send you a complimentary copy straight to your inbox!
.png?width=1200&height=630&name=nclex%20review%20for%20angina%20(2).png)
You CAN Do This
Happy Nursing!