INSULIN . . . Life Saver or Life Taker | How Insulin Works
.png)
Does insulin save lives, or does it take lives?
Bodies that don’t produce enough insulin shut down, but, if too much insulin is in the system, it can be just as disastrous.
As nurses, we are often tasked with administering insulin to our patients. When done incorrectly, it can be life-threatening.
For years I was a member of the code team, and countless calls happened because of failure to administer and monitor insulin dosages correctly.
A typical conversation would usually go something like this:
📢 Code Team: floor 1, bed 12, blood sugar is 20, patient unresponsive
Me: "When did you give them insulin?"
Them: "About 20 minutes ago."
Me: "When did you last check blood sugars?"
Them: "2 hours ago."
🏃Grab the crash cart and D50 and off we go…
It can be difficult to remember everything that is necessary to do, especially as a new nurse.
WHEN I was a new nurse, I vividly remember trying to keep track of my patients, insulin action times, dosage times, and everything in between. . .
I felt like I was drowning trying to keep it all straight in my head. . .
I was both stressed and scared at the same time.
THAT’S WHEN I copied all the insulin peak and onset times down in my notebook.
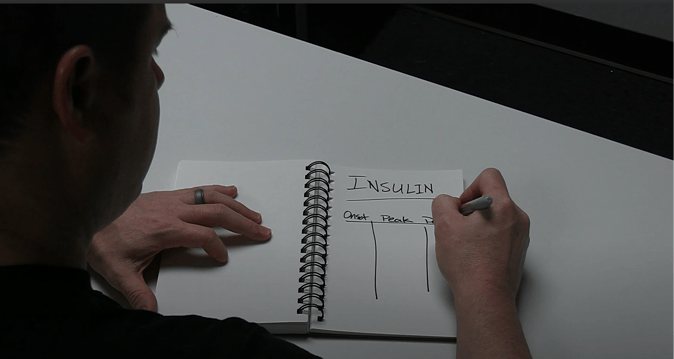
THIS HELPED me feel more relaxed because I knew I could reference them quickly to prevent my patient from coding!
Those notes are actually a full cheatsheet available on NURSING.com today. And you can have it for free if you want! You can download the cheatsheet at NURSING.com/cheatsheets.
Honestly, I still use the cheatsheet today.
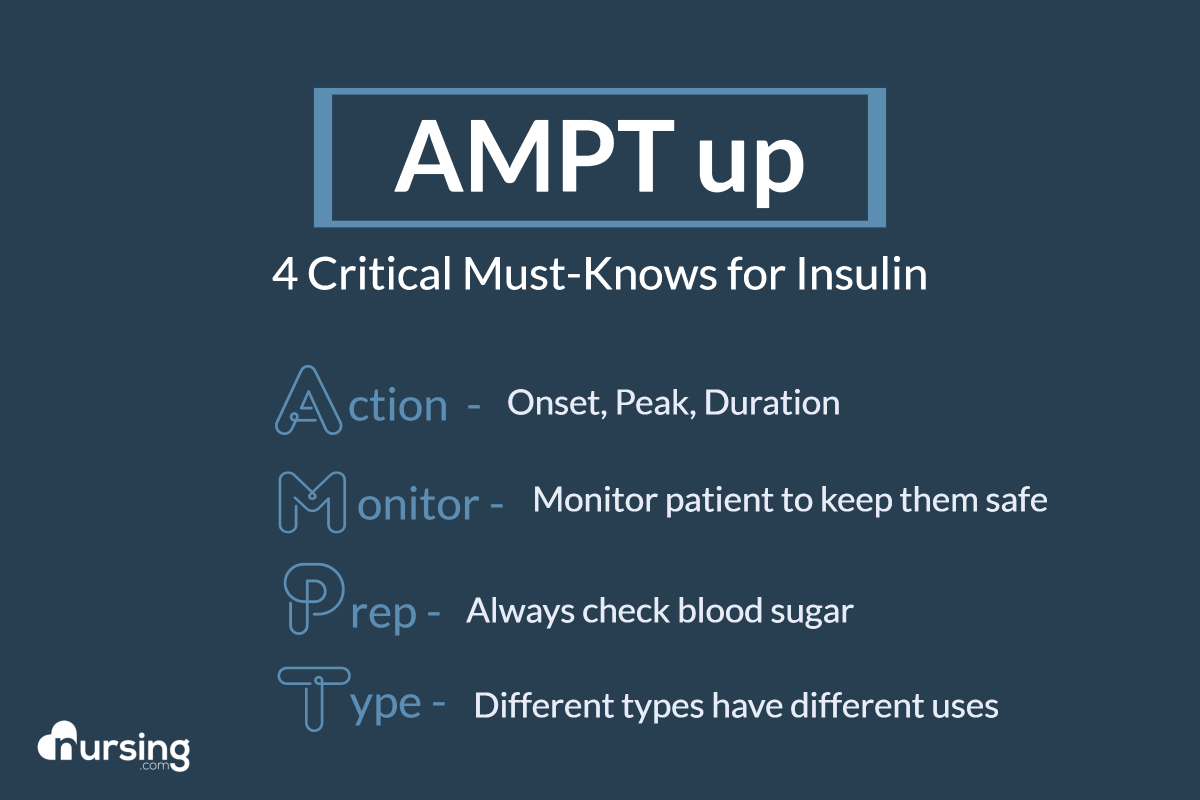
If you want to avoid causing an insulin-related critical code with one of your patients, I have an acronym that covers 4 Critical Must-Knows for Insulin:
AMPT up
If you want to master insulin as a new nurse, memorize AMPT up now, and you’ll be ready for that next insulin dosage!
- Action - Know the action of insulin in the body (hint: action differs with different types of insulin)
- Monitor - Know what to monitor to make sure your patient is safe
- Prep - Know what you need to do before you give a patient insulin
- Type - Know the different types of insulin and when they might be used
As we dig into our coding situation mentioned earlier, we will break down each of those “4 Critical Must-Knows for Insulin” along the way to piece it all together.
So let's talk about what happened in our coding scenario: why did that patient code and why can insulin be a lifesaver or a lifetaker?
A good analogy for describing insulin's role in the body is to compare it to a key that unlocks doors. Imagine that each cell in your body is a locked house. Glucose (sugar) is a package that is delivered to the "house" through the bloodstream and needs to get inside. Insulin is the key that unlocks the front door, allowing glucose to leave the bloodstream and enter the cells. Without insulin, the package would remain stuck outside, unable to deliver what is necessary for the cells to function properly.
Earlier I mentioned that the majority of emergencies for the code blue team came from insulin overdose. Why is that?
Continuing with the analogy of insulin being a key that unlocks doors for glucose packages to be delivered, if there is too much insulin, it's like having an overzealous locksmith who keeps opening the door and throwing in more packages!
As a result, there are not enough packages of glucose left in the bloodstream for other essential areas like the brain or heart.
.gif?width=1920&height=1080&name=Untitled%20design%20(1).gif)
That is when the patient becomes confused, possibly unresponsive, or worse.
Part of our role as nurses is to be aware of the interactions between insulin and blood sugar. so let's dig in and learn about insulin action in the body.
Our very first Critical Must-Know for Insulin is "A" for Action.
Action - Know the action of insulin in the body (hint action differs with the different types)
Insulin Action - Onset, Peak, Duration
When dealing with insulin and the interaction between insulin and blood sugar, this is referred to as onset, peak, and duration.
Getting the hang of insulin peak and onset times isn't just crucial; it's a lifesaver. Let's break down the basics to make your study sessions a breeze:
• Onset: refers to when insulin first starts to take effect in the blood.
For example, rapid insulin has a 15-minute onset after administration.
• Peak: when the insulin has its maximum effectiveness.
Looking at rapid insulin, that would be between 30 - 90 mins.
• Duration: refers to how long the insulin will have an effect.
For rapid insulin, it would be 3-5 hours.
Great . . . but how do we use these times? The goal is to time the insulin doses appropriately to the body's response to eating. When the patient eats carbs, they get an influx of glucose. We want to time the peaks of glucose in the blood with the peaks of insulin. Now just a quick note here: these onset, peak, and duration times will all vary depending on the type of insulin. But, don't worry! We will cover that for you, too, just a bit later.
A key to putting that all together is to know what to monitor in your patient.
Our next Critical Must-Know for Insulin is "M" for Monitor.
Insulin Monitoring
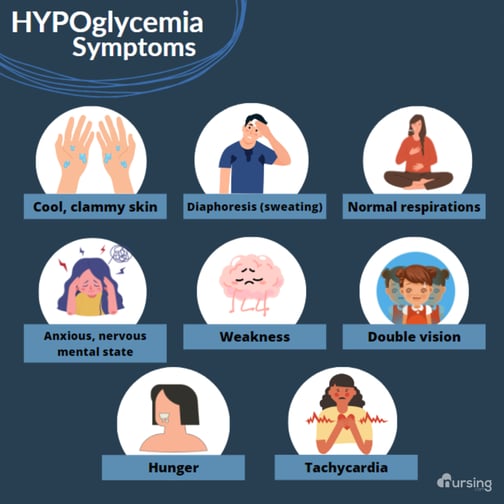
If we do not monitor our patients, the peaks of glucose in the blood and the peaks of insulin can get offset. Then we run the risk of our patients’ blood sugar crashing - you might find symptoms of shakiness, confusion, and weakness.

If the imbalance is not dealt with appropriately, then they can quickly go downhill even more.
Let's unlock the essentials of insulin monitoring together:
- Blood Sugar
- If we keep a close eye on our patients' blood sugar, we will know if our timing or amounts are off. The blood sugars will tell us because they will either go too high or too low.
- Symptoms
- Monitor your patient for any signs of adverse reactions
- Are they feeling dizzy, shaky, or experiencing sweating? It's vital to be attentive.
- Monitor your patient for any signs of adverse reactions
- Injection Site
- Rotate injection sites!
- This reduces the risk of lipodystrophy and ensures proper insulin absorption. It's a small step with a big impact.
- Rotate injection sites!
- Food
- Consider the timing of meals
- It takes about 15 minutes for consumed carbohydrates to start impacting the blood sugars. Blood sugars reach their highest about 1-hour post-prandial (after a meal) and usually return to normal after about 3-4 hours.
- Consider the content of meals
-
- Foods that contain only protein or fat have minimal impact on blood sugar
- Foods that contain carbohydrates will impact the blood sugars. Consider the type of food that your patient is eating.
-
- Consider the timing of meals
Matching insulin administration with meal schedules helps maintain stable blood sugar levels.
Next, we are going to discuss how you can best prep to give your patient insulin.
Our next Critical Must-Know for Insulin is "P" for Prep.
Prep - Know what you need to do before you give a patient insulin
Ever wonder what's the first critical step before giving insulin? It’s not what you might think!
The first step is crucial and often overlooked:
Always check the patient's blood sugar levels.

It directly influences the insulin dosage and type, tailoring the treatment to the patient's current needs with precision.
Getting an accurate reading is so important. It guides us in making informed decisions about insulin types — be it rapid-acting, short-acting, or others — and the exact dosage required.
I can't emphasize enough the absolute necessity of checking blood sugar levels accurately before administering insulin. And I don't mean any time before. It MUST be right before you administer insulin. If you wait an hour, you may misalign the peak of the blood sugars with the peak of the insulin. And, as we have discussed above, that is a recipe for disaster.
The last thing that we must cover is the different types of insulin, and then we will also include the onset, peak, and duration times for each insulin type as well.
Our next Critical Must-Know for Insulin is "T" for Type.
Insulin Types
Type - Know the different types of insulin, and when they might be used
Now let's review the different types of insulin and how they vary.
- First up, we have rapid-acting insulin
- Think of this as a magic turbo button on a race car - ZOOM, off like a flash. It helps the body handle sugar in a hurry.
.png?width=659&height=371&name=Simple%20Self-Care%20Blog%20Post%20Banner%20(1).png)
- Next in line, is short-acting, or regular insulin.
- It takes a little longer than rapid-acting to kick in. This would be like a mechanic performing the quickest tune-up to give the race car a sharp boost so it can continue in the race.
- Now, let's talk about intermediate-acting insulin.
- It has a more prolonged effect, providing a steady release over an extended period. This is like the intermittent pitstops for refueling throughout the race. It's not instant, but keeps the car functioning steadily.
- Next we have long-acting insulin.
- Picture it as a slow-release energy pack for the race car. It works gradually over many hours to help the body maintain stable energy levels for an extended period.
- Lastly, I want to discuss the very serious insulin drip.
- Continuous infusion of insulin directly into the patient's bloodstream. This impacts the blood sugar immediately and must be monitored closely.
- Continuous infusion of insulin directly into the patient's bloodstream. This impacts the blood sugar immediately and must be monitored closely.
** Insulin drip or insulin infusion is a medication that should be taken very seriously. Patients can quickly become hypoglycemic because they have insulin infusing in their IV continuously. Patients on an insulin drip must be in ICU. Some of the instances that a patient might be on an insulin drip include the following: diabetic ketoacidosis (DKA), postsurgical, or very critically ill patients. Not all of the patients on an insulin drip will be diabetics. In some cases, patients become hyperglycemic because of the stress their body is under with an illness or after surgery. They need to get placed on an insulin drip to quickly decrease blood glucose in a very controlled manner. With insulin drips, patients' blood sugars are checked regularly and the insulin is titrated (adjusted) very quickly in response to the patient's needs.
.png?width=2240&height=1260&name=Simple%20Self-Care%20Blog%20Post%20Banner%20(2).png)
Again, this is something that we want to do because people who have tighter glycemic control have better healing with surgeries or whatever illness they have. So it's, again, very common. When initiating the infusion, make sure that you follow the facility’s protocols - a set of instructions on what to do when you do start an insulin infusion.
Those were our types of insulin. Now lets look at the onset, peak, and duration times for the different types of insulin:
- First up, Rapid-Acting Insulin: starts working in 15 minutes, peaks around 30-90 min, and lasts 3-5 hours. Perfect for mealtime glucose control.
- Next, Short-Acting Insulin, or Regular Insulin: kicks in within 30-60 minutes, peaks between 2 to 4 hours, and holds the fort for 5-8 hours.
- Moving on to Intermediate-Acting Insulin: this one starts working in 1 to 2 hours, peaking at 6 to 14 hours, and lasts about 16-24 hours.
- Lastly, Long-Acting Insulin: is steady and reliable. It gets going in about 3-4 hours with a peak around 6-8 hours and lasts up to 24 hours. Another, called Glargine varies in onset, and tends to peak at 1 hour, lasting up to 24. And, lastly, Lantus, onset varies, peaks at 1 hour, and last 24 hours.
.png?width=1080&height=1080&name=INSULIN%20PEAK%20AND%20ONSET%20TIMES%20(2).png)
When I was in nursing school I realized mastering insulin administration isn't just about numbers; it's about ensuring every patient receives the best, personalized care.
I hope this can help you as it has me, to better understand insulin . . . and keep your patients as safe as possible.
Go out and be your best self today - Happy Nursing!