Did You Learn THIS About Fractures In Nursing School For Your NCLEX Review
Understanding Fractures
Understanding fractures is important for nursing students preparing for the NCLEX exam due to several reasons:
Common Occurrence: Fractures are a frequent occurrence, and nurses are likely to encounter patients with fractures in various healthcare settings. Knowledge about their types, causes, assessment, and management is crucial.
Impact on Mobility: Fractures can significantly affect a patient's mobility and independence. Nurses need to understand the implications of fractures on a patient's functional status and quality of life.
“What if I fail?”
You don’t need more questions. You need a real plan.
🎯 SIMCLEX + Flash Notes + ReadyScore = NCLEX Survival Package
Know you’re ready — before test day.
Assessment Skills: Nurses should be skilled in assessing patients with fractures, including evaluating the location, type, and severity of the fracture, as well as assessing for complications such as neurovascular compromise.
Pain Management: Fractures are often accompanied by significant pain. Nurses need to understand pain assessment techniques and various pain management strategies, including pharmacological and non-pharmacological interventions.
Immobilization Techniques: Nurses should be knowledgeable about various immobilization techniques, such as splints, casts, and traction, and their appropriate use based on the type and location of the fracture.
Neurovascular Assessment: Nurses play a critical role in monitoring neurovascular status distal to the fracture site to detect early signs of vascular compromise or nerve injury.
Complication Prevention: Nurses need to understand potential complications of fractures, including compartment syndrome, infection, and delayed healing, and how to prevent or manage them.
Patient Education: Nurses educate patients and their families about fracture care, the healing process, and the importance of following treatment plans and rehabilitation exercises.
Surgical Interventions: Nurses may encounter patients undergoing surgery for fractures. Understanding preoperative and postoperative care, as well as potential complications, is essential.
Emergency Management: In cases of open fractures or fractures with significant soft tissue damage, nurses should be prepared to provide immediate first aid and manage potential infection risk.
Documentation: Accurate documentation of the type of fracture, treatment provided, patient response, and complications is crucial for continuity of care.
NCLEX Preparation: The NCLEX exam may include questions related to fractures, their assessment, interventions, and patient education. A strong understanding of this topic is essential for answering these questions accurately.
Overall, understanding fractures equips nursing students to provide safe, patient-centered care to individuals with fractures. It ensures that nursing students are prepared to address the unique challenges and needs of patients with fractures and contribute to positive patient outcomes.
General Information for Fractures
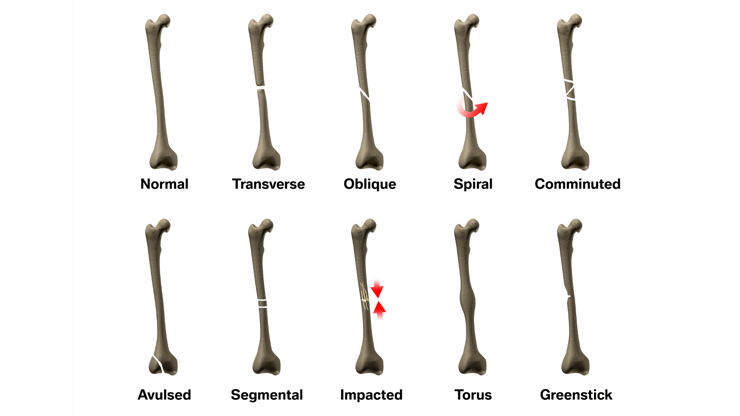
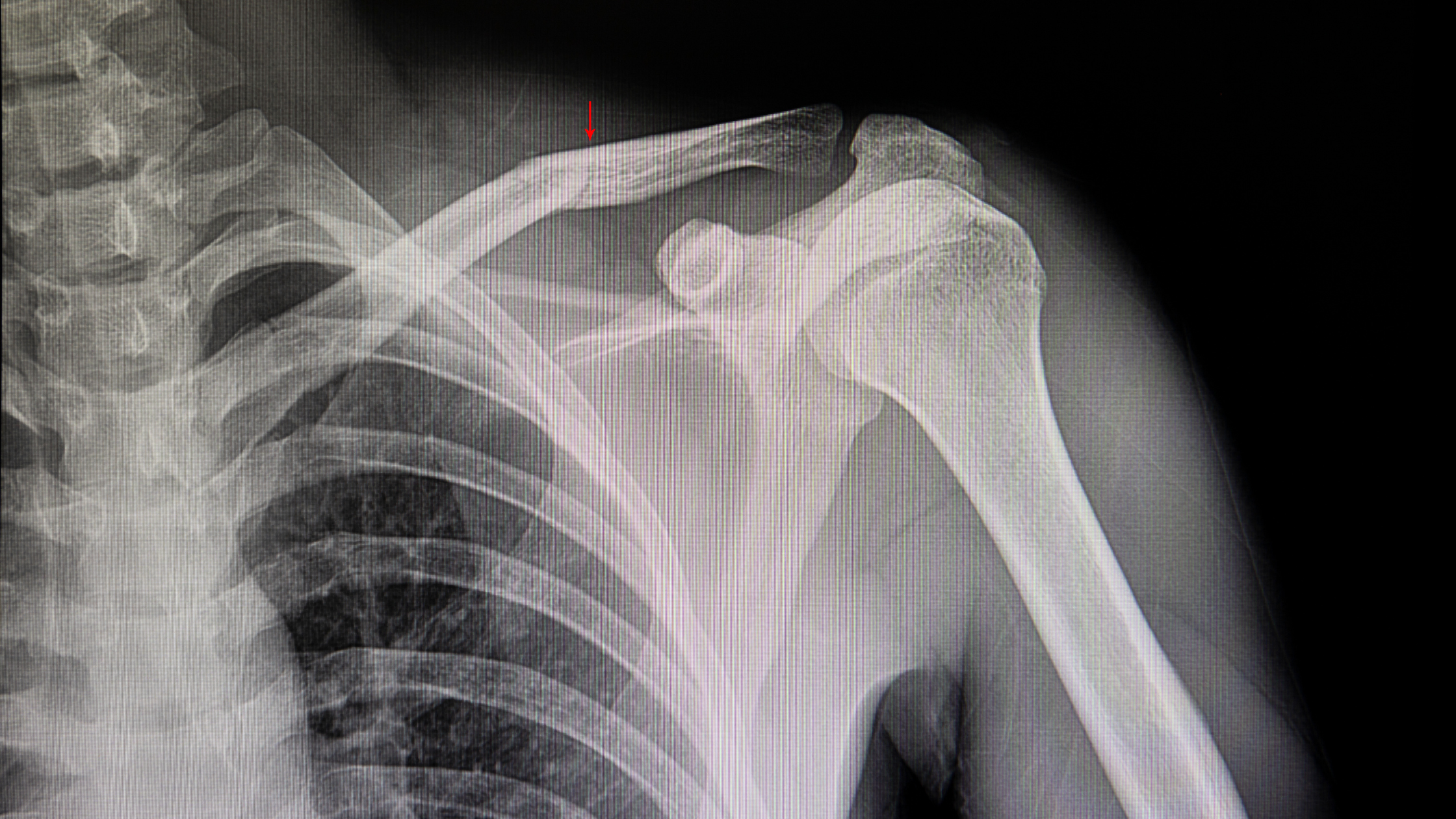
1. Types of fractures
a. Closed – skin intact
b. Open/Compound – bone pierces the skin
c. Transverse – broken straight across
d. Spiral – fracture from twisting force
e. Comminuted – multiple pieces of bone
f. Impacted – from the vertical force on long bone
g. Greenstick – incomplete fracture, common in children
h. Oblique – diagonal fracture
i. Displaced – bones no longer aligned
2. Strain
a. Excessive stretching of the muscle
3. Sprain
a. Excessive stretching of a ligament
4. Complications
a. Fat Embolism (when a piece of fat from bone marrow moves through the bloodstream to the lungs) is a risk with long-bone fractures.
b. Compartment Syndrome is when increased pressure within the compartment in the extremity after a fracture or crush injury cuts off circulation to muscles and nerves
Assessment for Fractures
1. Fracture
a. Assess distal circulation→ Pulses, skin temperature, color
b. Assess distal nerve function→ Numbness and tingling
c. May see ecchymosis over the fractured area
2. Fat Embolism
a. Anxiety, restlessness
b. Tachycardia, hypotension
c. Tachypnea, dyspnea
d. Petechial rash
3. Compartment Syndrome
a. Pale skin
b. Extreme swelling
c. Loss of pulses or sensation distal to the injury
Therapeutic Management for Fractures
1. RICE
a. Rest
b. Ice
c. Compression
d. Elevation
2. Cast
a. Stabilization of bone for healing.
b. Monitor extremities for:
i. Swelling
ii. Pain
iii. Discoloration
iv. Sensation
v. Circulation distal to cast
3. Traction
a. Force applied in the opposite direction to realign and immobilize the fracture
b. Ensure proper alignment of the body
c. Buck’s Traction – force applied to splint
d. Skeletal Traction – pin inserted through bone to hold traction force
e. Weights should hang freely from bed
i. Do not set them on the floor
ii. Do not remove weights without provider order
iii. Support weight when sliding up in bed
4. Fat Embolism
a. No specific treatment
b. Support hemodynamics
c. Corticosteroids
d. Monitor in ICU
5. Compartment Syndrome
a. Emergent intervention required to prevent loss of limb
b. Fasciotomy required to relieve pressure
Nursing Case Study for Fractures
Patient Profile:
John Miller, a 35-year-old construction worker, is brought to the emergency department after falling from a scaffold at a construction site. He complains of severe pain in his right thigh and is unable to bear weight on his leg. He has no significant medical history.

Assessment:
Upon assessment, John appears pale and is grimacing in pain. His right thigh is visibly swollen, and he has a deformity at the mid-shaft of his femur. Distal pulses are palpable, but capillary refill is delayed in the affected limb. He reports a tingling sensation in his right foot.
Interventions:
1. Neurovascular Assessment:
Perform a thorough neurovascular assessment, including assessing the pulses, color, temperature, and sensation of the affected limb.
2. Pain Management:
Administer prescribed pain medication to alleviate John's severe pain and make him more comfortable.
3. Immobilization:
Stabilize John's right leg using a splint to prevent further movement of the fracture site and minimize pain during transportation.
4. Diagnostic Imaging:
Collaborate with the healthcare provider to order X-rays to confirm the diagnosis, assess the extent of the fracture, and plan appropriate treatment.
5. Surgical Consultation:
Consult with an orthopedic surgeon to determine the need for surgical intervention to repair the femoral shaft fracture.
6. Preoperative Care:
Prepare John for surgery by ensuring he is NPO (nothing by mouth), starting intravenous fluids, and providing preoperative education.
7. Emotional Support:
Provide emotional support to John and his family, addressing their concerns and helping them cope with the situation.
8. Postoperative Care:
Collaborate with the surgical team to provide postoperative care, including monitoring vital signs, assessing wound status, and managing pain.
9. Mobility Assistance:
Assist John with safe mobility using a walker or crutches once he is cleared for weight-bearing.
10. Rehabilitation Referral:
Collaborate with physical therapy to develop a rehabilitation plan to help John regain strength and mobility in his affected leg.
11. Patient Education:
Educate John about the importance of adhering to the rehabilitation plan, maintaining follow-up appointments, and signs of complications.
Outcome:
Following surgical intervention and comprehensive care, John's femoral shaft fracture is successfully repaired. He undergoes a rehabilitation program and gradually regains strength and mobility in his right leg. With proper follow-up and adherence to the treatment plan, John returns to his previous level of function.
“What if I fail?”
You don’t need more questions. You need a real plan.
🎯 SIMCLEX + Flash Notes + ReadyScore = NCLEX Survival Package
Know you’re ready — before test day.
You CAN Do This
Happy Nursing!