The 3 P's of Diabetes Mellitus (DM) and why you should know them for your NCLEX Exam
The 3 Ps of Diabetes Mellitus
The 3 Ps
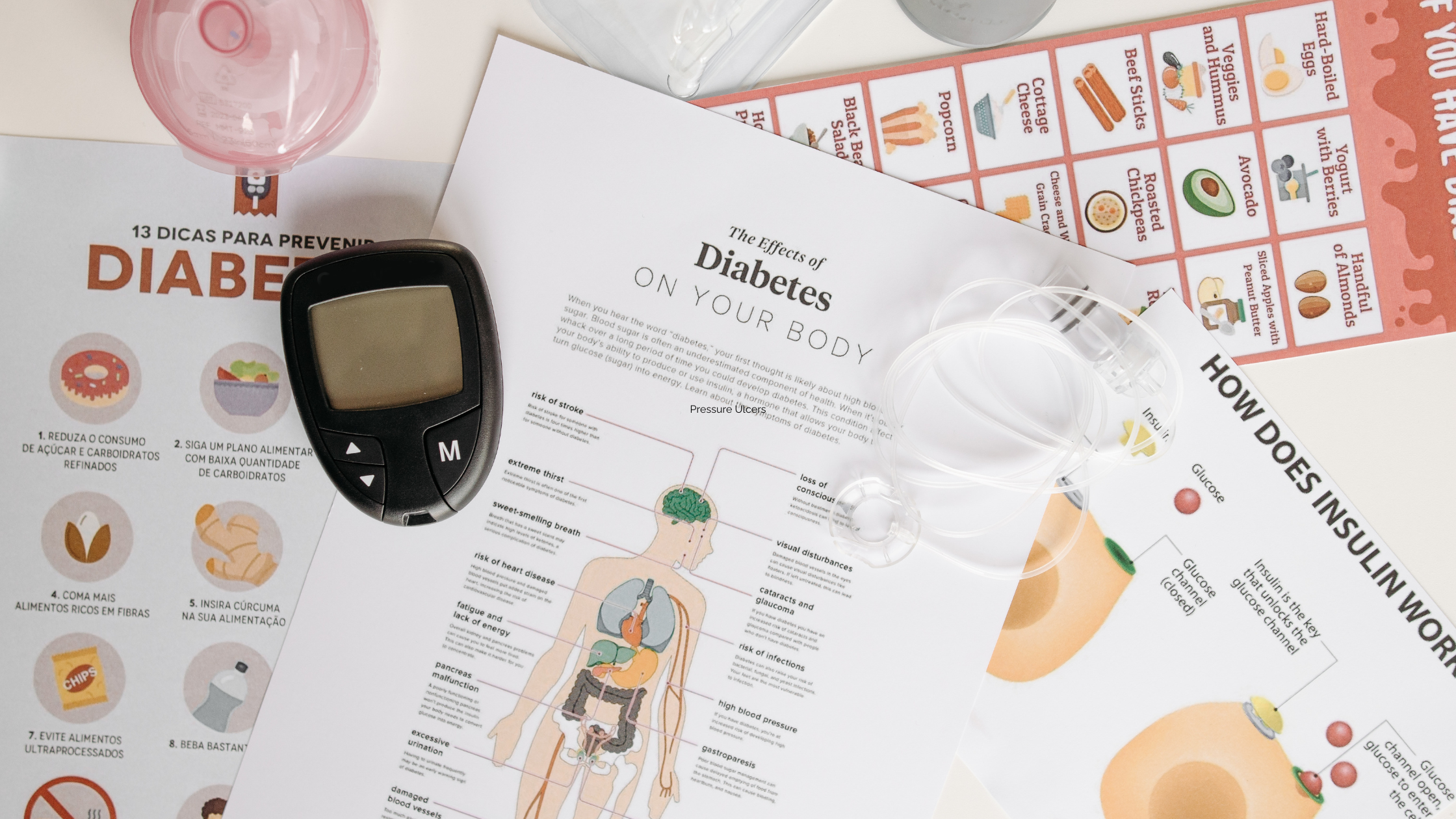
P-Polyuria (excessive urination)
P-Polydypsia (excessive thirst)
P-Polyphagia (excessive hunger)
In type 1 diabetes mellitus a patient does not produce insulin. Insulin allows glucose to go from the blood into the cells for energy. When glucose does not get into the cell, glucose levels in the blood rise. The body tries to remove excess glucose by producing extra urine. The body then requires more water. We get hungry because our cells are starving for energy.
Understanding Diabetes Mellitus is Crucial for Nursing Students:
High Prevalence: Diabetes Mellitus is a prevalent chronic condition worldwide. Nurses are likely to encounter patients with diabetes in various healthcare settings, making knowledge about its management and care essential.
Complexity: Diabetes Mellitus is a complex disorder with multiple types (Type 1, Type 2, gestational) and varying treatment approaches. Nurses need to understand the differences, causes, risk factors, and management strategies for each type.
Complications: Diabetes can lead to various complications, such as neuropathy, retinopathy, nephropathy, and cardiovascular disease. Nurses should be aware of these potential complications to provide comprehensive care and education.
Assessment Skills: Nurses need to be skilled in assessing for signs and symptoms of diabetes, including hyperglycemia, hypoglycemia, and related conditions like diabetic ketoacidosis (DKA) and hyperosmolar hyperglycemic state (HHS).
Medication Management: Understanding diabetes medications, including insulin, oral hypoglycemic agents, and injectables, is essential for nurses to ensure proper administration, monitoring, and patient education.
Blood Glucose Monitoring: Nurses play a vital role in teaching patients how to monitor their blood glucose levels, interpret the results, and adjust their medication and lifestyle based on the readings.
NCLEX Preparation: The NCLEX exam may include questions related to diabetes mellitus, its pathophysiology, assessment, interventions, and patient education. A strong understanding of this topic is crucial for answering these questions accurately.
Overall, understanding Diabetes Mellitus equips nursing students to provide safe, patient-centered care to individuals affected by this chronic condition. It ensures that nursing students are prepared to address the unique challenges and needs of patients with diabetes and contribute to positive patient outcomes.
Overview of Diabetes Mellitus
1. A pancreatic disorder resulting in insufficient or
lack of insulin production leading to elevated blood
sugar
2. Insulin is the “key” to allow glucose to enter cells
and be used for energy
General Information for Diabetes Mellitus
1. Type I
a. Autoimmune disorder
b. Body attacks beta cells in the pancreas
(responsible for insulin production)
c. The pancreas makes NO insulin, the client is
insulin-dependent
d. Ketosis due to gluconeogenesis (body making
glucose from fat cells), since it can not use
the glucose in the blood because the “key” is
missing
2. Type II
a. Beta cells do not produce enough insulin for the
body’s needs
b. OR – Body becomes resistant to insulin
c. Lifestyle-related
d. May or may not require insulin, depending on
the severity
Assessment for Diabetes Mellitus
1. Vascular and Nerve Damage
a. Related to inflammation and hyperosmolarity in
vessels
b. Poor circulation→ because the blood is thick
with glucose
c. Poor wound healing
d. Retinopathy → blurry vision
e. Neuropathy → decreased sensation, especially
in feet/toes
f. Nephropathy → may result in Chronic Kidney
Disease
2. The Three P’s
a. Polyuria
b. Polydipsia
c. Polyphagia
3. Elevated HgbA1c > 7.0
a. A measure of the average blood sugar over the
last 3 months
4. Complications
a. Dawn Phenomenon→ Reduced insulin
sensitivity between 5-8am that can be helped
with evening insulin administration
b. Somogyi Phenomenon→ Nighttime
hypoglycemia results in rebound hyperglycemia
in the morning hours, which can be helped with
a bedtime snack
c. Diabetic Ketoacidosis (DKA) → Acute
exacerbation of Type I Diabetes Mellitus
(hyperglycemia resulting in the spilling of sugar
into the urine)
d. Hyperglycemic Hyperosmolar Nonketotic
State (HHNS) → Acute exacerbation of Type II
Diabetes Mellitus ( Caused by increased blood
sugar levels which leads to ↑ osmotic pressure
in vessels → cellular dehydration)
Therapeutic Management for Diabetes Mellitus
1. Oral Antidiabetic Agents
a. For Type II Diabetics
b. Glucophage (Metformin) = most common
c. Glipizide (Glucotrol)
2. Insulin
a. Required for Type I
b. Type II may require insulin if diet, exercise, and
oral antidiabetic agents aren’t enough
c. Most at risk for hypoglycemia during insulin
peak times
d. ONLY Regular insulin can be given by IV
e. Mixing Regular and NPH
i. Clear before Cloudy
ii. Inject the air into cloudy → Inject the air
into clear and draw up clear → draw up
cloudy
iii. Avoids cross-contamination or errors in
drawing up
f. “Insulin Reaction” → hypoglycemia
i. Cool, clammy, diaphoretic
ii. 15-15 Rule: Give 15 g sugar (4 oz. juice or
soda) and recheck in 15 minutes
3. Diet and Exercise
a. May improve insulin response for Type II
Diabetics AND can help stabilize blood sugars
in Type I Diabetics.
.png?width=1200&height=630&name=nclex%20review%20for%20angina%20(2).png)
Nursing Case Study for Diabetes Mellitus
Patient Profile:
Sarah Thompson, a 55-year-old woman, is admitted to the hospital with complaints of fatigue, frequent urination, and unexplained weight loss. She has a family history of diabetes and is overweight. Her blood glucose level is significantly elevated.
Assessment:
Upon assessment, Sarah appears fatigued and reports feeling thirsty. She mentions needing to use the bathroom frequently, even during the night. Her body mass index (BMI) indicates she is overweight. Her blood pressure and cholesterol levels are also elevated.
1. Blood Glucose Monitoring:
- Teach Sarah how to monitor her blood glucose levels regularly and interpret the results.
- Collaborate with a registered dietitian to provide Sarah with personalized nutritional guidance to promote glycemic control and weight management.
- Collaborate with the healthcare provider to initiate oral hypoglycemic medications to help lower Sarah's blood glucose levels.
- Educate Sarah about the importance of regular physical activity and weight reduction to improve insulin sensitivity.
- Educate Sarah about the significance of proper foot care and how to perform regular foot assessments.
- Collaborate with the healthcare provider to initiate antihypertensive medications and provide education on the importance of blood pressure control.
- Educate Sarah about the signs and symptoms of hypoglycemia, how to manage it, and the importance of adhering to her medication regimen.
- Educate Sarah about the potential complications of diabetes, such as neuropathy, nephropathy, and retinopathy, and how to reduce her risk.
- Provide emotional support to Sarah, addressing any concerns or fears she may have about managing her condition.
- Schedule regular follow-up appointments to monitor Sarah's blood glucose control, adjust medications as needed, and assess her progress.
Outcome:
With comprehensive care and patient education, Sarah's condition improves. Her blood glucose levels gradually normalize, and she experiences increased energy and improved well-being. She becomes educated about diabetes management and embraces lifestyle changes to better manage her condition.
Free Download
Are you looking for more must-know NCLEX review topics? Download our free eBook "NCLEX Flash Notes" as a valuable resource for nursing students. Encourage readers to download their free copy of the "NCLEX Flash Notes."
.png?width=1200&height=630&name=nclex%20review%20for%20angina%20(2).png)
You CAN Do This
Happy Nursing!