What I Wish I Knew: A Patient With Coronary Artery Disease (CAD
.png?width=186&height=186&name=Copy%20of%20Copy%20of%20Minimalist%20Planner%20Pages%20Mockup%20Instagram%20Post%20(5).png)
“I would rather go to the hospital and have them
tell me it's indigestion than die at my desk“
- Todd
Meet Nurse Jon
I’m Jon, RN, CCRN Alumnus!
 One of my favorite rotations was when I had the opportunity to work in the ER because you just never know who’s going to come in through those doors…
One of my favorite rotations was when I had the opportunity to work in the ER because you just never know who’s going to come in through those doors…
And patients with heart issues. . those were always tricky!
As tricky and complex as the heart is, though, it’s not impossible to grasp those critical aspects of how it works, what happens when it malfunctions, and what you need to do as a nurse to provide the best care for your cardiac patients. If you need some help, I’ve got you covered - go to nursing.com/heart to learn more!
One afternoon I got a phone call from Todd - our content director here at NURSING.com.
Hey man, so uh, just letting you know that I’m at the hospital being admitted. I’m having a heart attack, so I probably won’t be in tomorrow.
Now let's meet Todd
Just a little background: Todd’s 47 years old, doesn’t drink, has never done any sort of recreational drug, doesn’t smoke, and has been a vegetarian for 25 years.
Many would consider that to be pretty healthy - Todd thought so, too. . .
But, as Todd will tell you below . . . sometimes. . . that doesn’t matter:
I was sitting at my desk drinking coffee as usual and I started feeling a dull cramping chest pain, dead center of my chest.
It was like nothing I’ve ever felt before.
I've had lots of pulled muscles in my life, so I found it a little odd.
I thought maybe it was an air bubble, so I walked around the house, swinging my arms, jumping around, and moving my legs. But that only made it worse.
So, I laid down for a minute, but that made it worse, too.
Keep in mind, this was all in the course of about 15 minutes.
Coronary Artery Disease Symptoms
After that time, and because it was only getting worse no matter what I did, I started googling - as everyone does - and I landed on the American Heart Association’s website and started reading about heart attacks.
I was looking over the symptoms and man, it was like a checklist of all that I was experiencing: chest pain (obviously), numbness/tingling in my fingers, pain in the back of my neck. . .
The only 2 symptoms listed on the website that I wasn’t experiencing were nausea and cold sweats.
So I went downstairs to ask my wife to take me to the hospital because I thought to myself, I would rather go to the hospital and have them tell me it's indigestion than die at my desk.
I couldn’t find my wife inside so I went outside to look for her and BOOM - cold sweats popped out of nowhere and the chest pain was INTENSE.
It was at that moment - I knew. I knew what was happening.
When I found her, I calmly asked her if she could drive me to the ER.

When we got to the ER and I told them what was happening, they bumped me in front of everyone - like I didn’t even fill out any paperwork at all.
Coronary Artery Disease Diagnosis
They hooked me up to an EKG and elevation in the ST segment verified that I was having a heart attack.
They put an IV in me, gave me a chewable baby aspirin and a nitroglycerin tablet and my blood pressure dipped - I got really faint and pale and I started sweating profusely.
They suspected I may have had a blocked artery but they didn’t have a Cath Lab on site, unfortunately, so they took me by ambulance to a nearby hospital about 15-20 mins away.
Once at the other hospital, they wheeled me straight into the Cath Lab and nurses immediately got to work.

The plan was to inject some dye into my heart to see if there was a blockage and, if so, see where the blockage was.
Once the dye was injected, the doctor looked up at one of the screens, and showed me my whole heart with the dye, and said, “you’ve got a blockage in one of your arteries. We are going to clear that for you”
Did you correctly guess the cause of Todd's symptoms? Click below to take a FREE quiz on coronary artery disease. See what your current level of understanding is. Click below to try it!
Go ahead, I’ll wait . . . just click here.
How did you do?
Now back to the story…
Coronary Artery Disease Treatment
They told me they were going to go up through my wrist into that blocked artery and inflate a balloon to open the artery, and leave a mesh stent to keep the artery open and clear of blockage.
The worst part of that procedure was when they dilated the blocked artery in my heart . . . I started sweating so much again, the nurse had to keep drying me off and it felt like an elephant was on my chest.
At one point, the pain was so intense, I really thought I was dying.
I voiced my worry out loud, and they said that everything was okay - it was normal to feel that way.
When they opened the blockage, all the blood perfused back to my heart causing that weird intense feeling. The best way I can describe it is kind of like when your arm falls asleep and it hurts when the blood starts flowing back into the muscle.
The whole procedure was about 15-20 minutes and they put a plastic cuff over my radial artery (insertion point) where they went in and filled the cuff with air to create pressure, so that I wouldn’t bleed out and they rolled me back into a recovery room.
The biggest question that was rolling around in my head was: how could this have happened??
Coronary Artery Disease Prevention
They asked me about my family history and that’s where I found part of my answer: genetics
My family has a history of CAD, high BP, high cholesterol, & A-Fib
I definitely took it up a notch with a straight-up heart attack, but they told me it is somewhat a genetic issue.
The nurses told me that just the day before I came in, there was a 28 year old triathlon runner getting a stent put in, too.
My first thought was, “I'm an overweight failure that eats too much Taco Bell and pizza and this is all my fault.”
.gif?width=456&height=456&name=Copy%20of%20Copy%20of%20Minimalist%20Planner%20Pages%20Mockup%20Instagram%20Post%20(1).gif)
So, it felt good to know that it happens to other people that are otherwise healthy and on the young side.
That being said, plaque buildup does happen as a result of a lifestyle habit, too, so the day I got out of the hospital, I went vegan.
I gave up most of what I like to eat, I even cut out coffee for a while but I don’t like to talk about that - it’s still a sore topic.
I was dedicated to doing my 6-week cardiac rehab and completed it successfully.
My doctor said, “yeah, you’ve got CAD, but with your dietary changes and with you having successfully completed your rehab, I am not too worried. You should be able to live well into your eighties.”
I think there’s about a 40-45 minute window between when your heart attack happens and when it needs to be addressed before there’s any permanent damage to the heart muscle and, luckily for me, I made it within that window and didn’t have any permanent damage so I feel very fortunate.
I feel grateful that I didn’t think twice about getting it checked out, and I’m even more grateful for the rapid response of the ER nurses and the nurses in the Cardiac Unit.
The doctors were great, but the person that met me in the ER and worked quickly to hook me up to an EKG was a nurse and the first person that knew I was having a heart attack was a nurse.
They kept me calm and joked with me in a situation that was literally life-threatening.
I already appreciated nurses as it was but now. . .they literally saved my life.
So let's talk a bit more about CAD, and what was happening with Todd.
Coronary Artery Disease Pathophysiology
Let’s quickly recap on what happened in Todd’s arteries, how those symptoms presented, why it happened (and other potential risk factors), and why the quick actions of the nurses and medical staff were the right actions that saved Todd’s life.
As we said earlier, CAD is the narrowing or blockage of coronary arteries (atherosclerosis) due to plaque buildup. Atherosclerotic plaques build up on the artery walls, reducing blood flow to the heart muscle which can lead to angina (or chest pain), myocardial infarction (heart attack), and other cardiac complications.
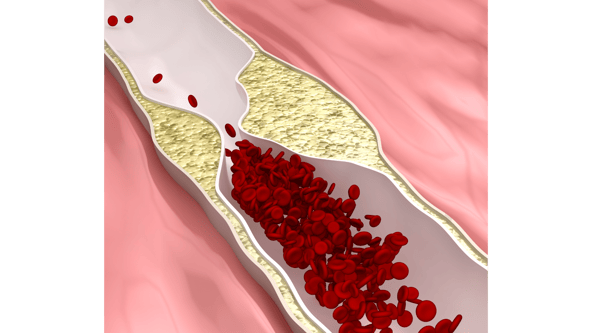
Let’s look at this picture of a normal vessel: the opening is wide and clear, allowing oxygenated blood to flow freely.
When CAD starts to develop, the vessel wall is damaged and scar tissue forms which thickens the vessel, creating a much more narrow pathway for blood to pass through.
Plaque from fats/lipids in the blood starts to stick to the wall of the vessel, then, a chunk of plaque breaks off.
When this happens, the blood goes through a clotting process around that chunk of plaque which makes the chunk even chunkier.
As it keeps moving through the bloodstream, it gets stuck due to the plaque on the vessel walls causing an occlusion which cuts oxygen perfusion to the heart muscle.
If the heart cannot get that oxygenated blood, then the heart muscle starts to die, which could ultimately lead to cardiogenic shock or heart failure.
So now the presentation of how CAD manifests itself:
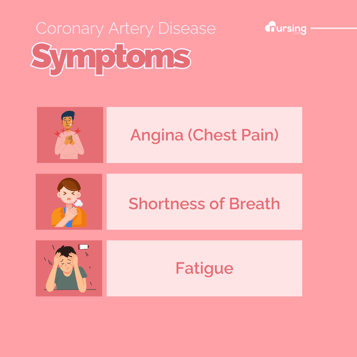
CAD Symptoms
Sometimes, there are NO symptoms until the patient has an MI or heart attack, or experiences angina.
However, IF patients do exhibit symptoms, they could show up as:
- Chest Pain (or Angina) which may radiate to the left arm
- Arrhythmia
- Shortness of breath
- Fatigue
- Dizziness
- Elevated BP
.png?width=356&height=356&name=Coronary%20Artery%20Disease%20Symptoms%20(1).png)
In Todd’s case, he had been feeling tired and easily winded but didn’t think it was anything more than him getting old.
CAD Risk Factors
Now the WHY: As Todd’s story shows, one reason CAD can occur is due to genetics - it runs in the family.
Other risk factors include:
- High BP
- Smoking increases blood pressure, and damages vessels making an oasis for plaque build-up
- Excess weight because there are typically higher levels of fat/lipids in the blood
- Diabetes because it causes inflammation and disrupts blood viscosity and therefore, blood flow
- Hyperlipidemia because of buildup of fat/plaque in the vessels
So as seen by these risk factors, apart from genetics, lifestyle habits also play a major factor in whether someone is at risk for CAD.
Lastly, let’s talk about the right actions/interventions the medical staff took to save Todd’s life:
CAD Interventions
Time is of the essence in a situation like Todd’s.
The nurses taking him back immediately upon arrival, knowing the details of what he was experiencing, was 100% crucial to the outcome Todd had. It’s said, “Time is muscle,” and it’s very common for hospitals to adhere to a standard of getting the patient to the cath lab in 90 minutes or less when an MI is suspected to reperfuse the heart muscle as quickly as possible to lower mortality.
Hooking him up to an EKG was another accurate intervention by the nurse.
When looking at the EKG, the nurse was probably looking for an elevation in the ST segment.
.jpg?width=536&height=299&name=ST_elevation_myocardial_infarction_ECG_(cropped).jpg)
Various, CC BY 4.0 <https://creativecommons.org/licenses/by/4.0>, via Wikimedia Commons
The EKG helps identify what type of ischemia the patient may be experiencing like:
STEMI which is near or complete blockage, and shows ST elevation, as the acronym is “ST elevation MI”
NSTEMI which is a partial blockage, but will not show ST elevation on EKG and. . .
Unstable angina which also can exhibit abnormalities on EKG due to ischemia
After their diagnosis of a heart attack as shown on the EKG, they administered a chewable baby aspirin and a nitroglycerin tablet.
Nitroglycerin is a vasodilating medication, which relaxes the muscle of blood vessels, creating vasodilation to lower blood pressure and improve blood flow.
Based on the EKG, they suspected a blockage was the cause behind the MI but since they didn’t have a Cath Lab to perform an angiogram, they transported Todd to a facility that did.
Once there, they performed fluoroscopy by injecting contrast dye into Todd’s blood vessels and performed an angiogram to see how bad the blockage was and where it was located.
When it was located, they performed a coronary angioplasty which involves a mesh stent being inserted through a tube into the blocked artery.
Once in the artery, the balloon is inflated, which does temporarily block the artery completely. But when it’s deflated, and the stent is in place, the blood flow wooshes through quickly especially since the blockage is cleared.
Which is why Todd felt like he was dying! The pain he felt was due to reperfusion of part of the cardiac muscle that had been blocked.
So there’s the what, how, why, and right actions/interventions the medical staff took to save Todd’s life.
But Todd also took measures to save his own life post-heart attack.
The biggest hurdle was unblocking his artery, obviously, but continued care for his overall cardiac health is needed as he is genetically predisposed to cardiac issues.
He went to cardiac rehab regularly for those 6 weeks and he made dietary changes as well. As much as they hurt him. . . like giving up his beloved coffee for several weeks to reduce caffeine in his diet, which is a stimulant but his heart needed rest.
So Todd is doing his part to make sure the chances of this happening again are slim.
I stressed about passing my class and ultimately passing the NCLEX.
I found success when I started using NURSING.com because it helped me find the must-know information with clear and concise videos, and then I would check my knowledge with the lesson quizzes.
I used the SIMCLEX to not only evaluate if I was ready for the NCLEX, but it would also give me personalized suggestions on what I should study to fill in my knowledge gaps.
I could focus on those topics further with custom quizzes as well as using the additional study tools that are adapted to my personal learning style.

If you are still looking for those moments where everything clicks and you start to think like a nurse. . . what worked for me was NURSING.com - and for more specifically on the heart you can go to nursing.com/heart.
Now, to help build your coronary artery disease knowledge we have pieced together the beginnings of a CAD care plan.
Coranary Arter Disease CAD Care Plan
Coronary artery disease is a common condition you will deal with working as an RN. Let me share part of my care plan with you, that I would use to help a patient with coronary artery disease.
Let’s start with the desired outcomes for the patient
Desired Outcomes for Coronary Artery Disease Nursing Care:
- Reduction or control of symptoms like angina.
- Improved or maintained cardiac function.
- Effective management of risk factors.
- Enhanced understanding and adherence to a healthy lifestyle.
- Patient reports of chest pain or discomfort (angina).
- Shortness of breath, fatigue, or dizziness.
- Concerns about lifestyle changes and disease management.
Objective Data:
- Physical examination findings (e.g., blood pressure, heart sounds).
- History of risk factors for CAD (e.g., hypertension, smoking).
- Laboratory results showing lipid profiles, blood glucose levels.
- Electrocardiogram (ECG) or stress test abnormalities.
- Imaging studies like angiography showing coronary artery blockages.
Nursing Assessment for Congestive Coronary Artery Disease:
- Assess for signs and symptoms of myocardial ischemia.
- Evaluate the patient’s understanding of CAD and its management.
- Monitor for complications, such as heart failure or arrhythmias.
- Assess lifestyle factors contributing to CAD.
Nursing Interventions and Rationales for Coronary Artery Disease
Evaluation for Coronary Artery Disease Nursing Care:
.png?width=2240&height=800&name=Copy%20of%20Header%20Banner%20for%20Blog%20(2).png)
The entire CAD Care Plan - along with 230+ other care plans - is available on NURSING.com.
Looking for more? Visit NURSING.com/heart now to download a Nursing cheat sheet for free.
I hope this has helped you understand coronary artery disease a bit better so you know what to look out for.
We’re rooting for you . . . Go out and be your best self today. . .
Happy Nursing!



.png?width=589&height=589&name=Minimalist%20Planner%20Pages%20Mockup%20Instagram%20Post%20(2).png)
-1.png?width=352&name=Untitled%20design%20(5)-1.png)

.png?width=352&name=Coronary%20Artery%20Disease%20nclex%20review%20for%20nursing%20students%20(1).png)